 |
Q:
A 62-year-old male presented two weeks after cataract surgery in his left eye for surgery in his right eye. While the one-day and one-week postop visits performed by his optometrist were perfect, with good vision and white, quiet eyes, my exam revealed sectoral injection nasally in the left eye. Could this be episcleritis, or something else related to surgery?
A:
“Sector injection almost always leads the clinician to a diagnosis of episcleritis,” says Jessica Kenney, OD, an ocular disease resident at Omni Eye Services of Atlanta. While episcleritis is certainly high on your list of differentials for sector injection, she says, it should be entertained only after ruling out other entities, especially conjunctival abrasions. These are quite common, but often go undetected in the search for something more interesting, such as episcleritis, Dr. Kenney says.
A patient with a conjunctival abrasion may present asymptomatically, as is the case with this patient, or with tearing, pain and general discomfort. Patients with episcleritis may also be asymptomatic, aside from noticing their eye is red. Pain is rare, but they may notice some irritation and watering as well. A detailed history is critical, and often patients’ initial answers don’t reveal the truth, so clinicians have to dig a little deeper.
 |
| Sectoral injection after cataract surgery isn’t always episcleritis. |
Differentials
Always look at Staph. lid disease as a common cause of chronic injection, Dr. Kenney says, as it can mimic a number of other entities and can cause asymmetric patterns of injection. Other differentials for sector injection include inflamed pinguecula, pterygium, subconjunctival hemorrhage, lodged foreign body and scleritis, all with their own unique appearance and characteristics, according to Dr. Kenney. In this patient’s case, clinicians can even consider a rebound iritis from the cataract surgery, although the injection is usually diffuse, not sectoral.
Often, when patients are not forthcoming with their history, objective findings outweigh the lack of confirmatory history. Dr. Kenney recommends clinicians make the proper treatment call based on the slit lamp exam, which will be grounded in the objective findings.
The Real Story
Dr. Kenney saw this patient prior to his right eye surgery, after the patient’s wife mentioned the red left eye to a staff member. The examination revealed sectoral injection nasally in the left eye, with a clear cornea and no anterior chamber reaction. The patient reported an unremarkable history and “nothing out of the ordinary” around the time he noticed the redness.
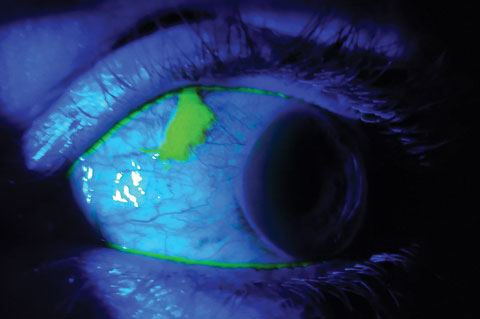 |
| Fluorescein revealed a conjunctival abrasion. |
But Dr. Kenney jogged his memory by inquiring about specific activities, such as working in the yard or other outdoor activities, and he recalled chasing after his dog into some brush when a branch hit his eye. “When I examined the nasal aspect of his eye, the conjunctiva had an elevated, clumped, milky appearance, which caused me to generously instill fluorescein into the eye,” Dr. Kenney explains. “The area stained perfectly and revealed what was already suspected—a conjunctival abrasion.”
The patient was put on a topical fluoroquinolone drop four times a day, and at the one-week follow-up visit, his referring optometrist reported that he was doing well, with resolution of the injection in his right eye and a quiet anterior segment. “If we had jumped to the first and seemingly most obvious diagnosis of episcleritis, we would have used a steroid that would most likely have delayed healing, not enhanced it,” says Dr. Kenney. “Keep an open mind and get the big picture while running through all possible differentials on every patient.”

