 |
Q:
I have a chronic herpes simplex patient with significant epithelial keratitis who might be resistant to acyclovir. Compliance does not appear to be an issue, but Valtrex along with steroid use is no longer helping. How can I be certain there is resistance? If there is, what is the best approach?
A:
Managing herpes simplex of the eye is mediated by frequency of occurrence and relative risk of vision loss over time, according to Jim Thimons, OD, medical director and founding partner of Ophthalmic Consultants of Connecticut. Of the possible treatments, Dr. Thimons says chronic oral therapy can help mitigate vision loss from tissue damage over time. Long-term therapy, however, can pose potential problems.
Because patients are living longer, they are receiving oral antiviral therapy for extended periods of time, Dr. Thimons notes. He adds that some could be on therapy indefinitely. As such, the rate of resistance to treatment has been slowly but steadily rising.
“With increased utilization, it is inevitable that the effect of the drug on the disease state is probably going to be altered,” Dr. Thimons adds.
Regardless, Dr. Thimons notes that the majority of immuno-competent patients—those who have herpes simplex keratitis but are healthy otherwise—have significant and persistent responses to acyclovir, the primary agent against which all sensitivities are tested. Resistance is rare in these patients—more than 99% are sensitive to the drug, according to Dr. Thimons. Immuno-incompetent patients, on the other hand, develop resistance to treatment the longer it is administered, and they do so at a much higher rate, Dr. Thimons says.
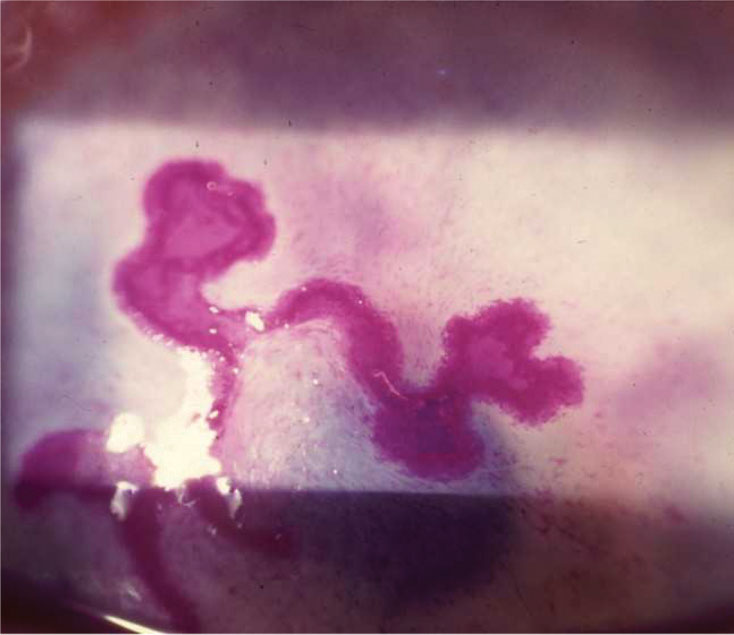 |
Pictured here is a large dendrite with end bulbs that are stained with rose bengal. |
A Mutating Case
Resistance usually develops due to mutations in the thymidine kinase pathway that cause patients to become non-sensitive to acyclovir and its pro-drug valacyclovir, according to Dr. Thimons. He adds that these mutations occur randomly in immuno-competent patients but can be predicted by the severity of the disease state in immuno-incompetent patients.
Response to a Rarity
In this particular case, the prescriber followed the appropriate treatment course but ran into a rare situation, says Dr. Thimons, who offers several treatment recommendations moving forward. His first suggestion is switching the patient from acyclovir to famciclovir or topical ganciclovir, both of which do not belong to the same family as acyclovir and contain different molecules that the patient could be sensitive to, he notes. Dr. Thimons also recommends ODs consider the use of “old school drugs” like trifluridine and vidarabine, which are less effective than current oral agents but play an active role in managing viral infectious processes, he notes. He adds that these drugs have different mechanisms of action, so patients might be more sensitive to them.
According to Dr. Thimons, the solution to this problem could be as simple as switching medications, but he warns doctors not to wait too long or else they could risk the chance of glaucoma developing in their patient. If new drugs are administered but are not effective within a week or two, Dr. Thimons advises referring to a corneal specialist for cellular analysis to determine what type of mutation is present and, from there, what path to take for the most successful results.

