 |  |
Concretions—calcified deposits embedded within the palpebral conjunctiva—are often small and do not cause irritation. However, if they are large or prominent, they may rub against the bulbar conjunctiva or cornea, resulting in irritation, pain and foreign body sensation. For these, clinicians should consider surgical excision for immediate relief.
Presentation
Concretions are often an incidental finding during anterior segment evaluation. They are more prevalent with age and in those with chronic inflammation. They appear as small yellow or white deposits that are usually less than 1mm. These deposits arise from epithelial cells, protein, mucin and other debris trapped in the fornix that calcifies over time.1 Concretions are most commonly located in the inferior palpebral conjunctiva.1,2
Patients with concretions are often asymptomatic and usually only require observation. But large or elevated concretions, especially in the upper lid, are more likely to rub the bulbar conjunctiva or cornea during the blinking process. These patients may complain of irritation and a foreign body sensation. In these cases, the concretions should be removed surgically for patient comfort.2
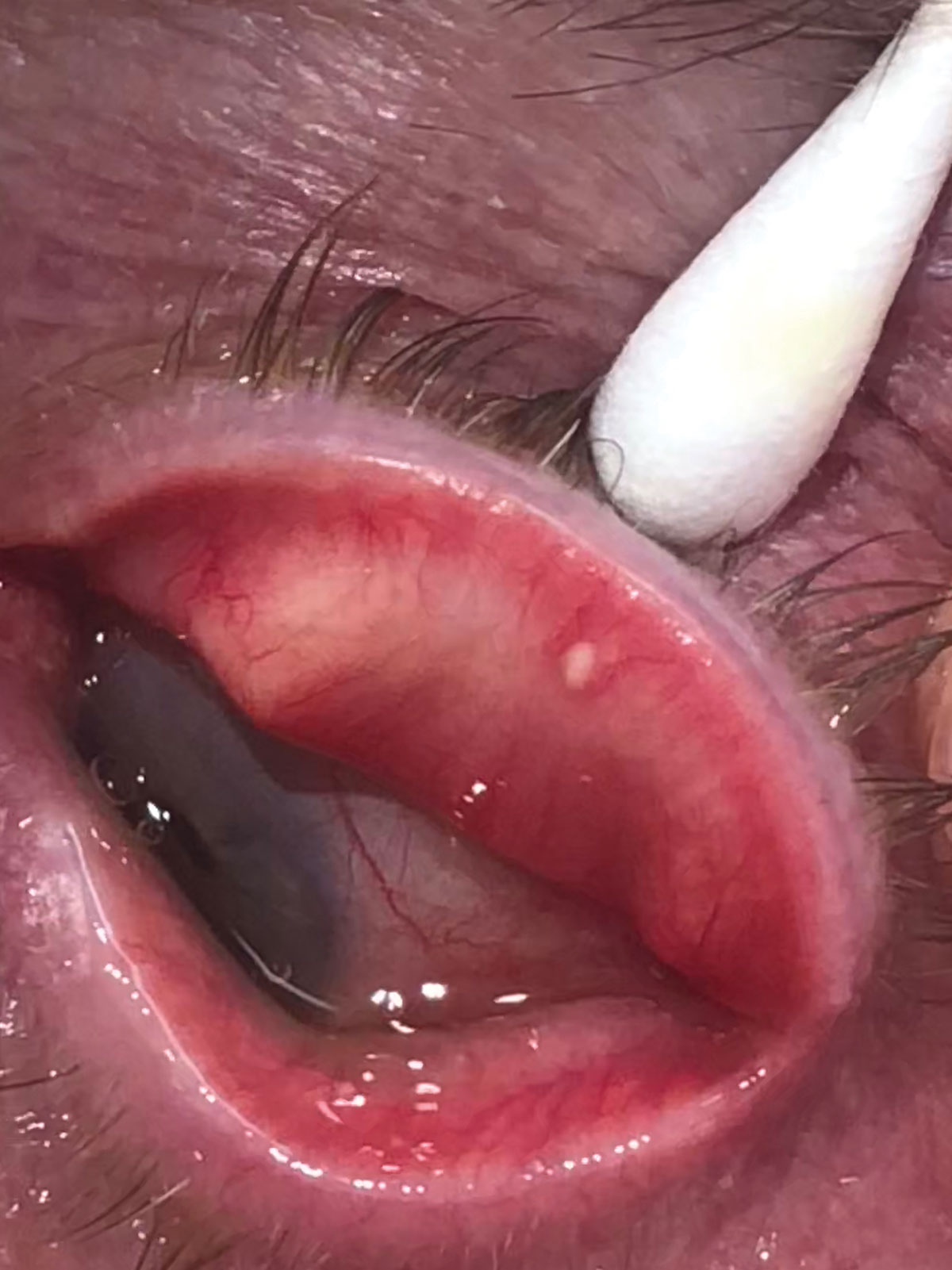 |
| Palpebral view of concretion near the lid margin. |
Excision: Step-By-Step
Removal is typically performed under local anesthesia using no sedation. The patient is placed in a supine position, and lidocaine hydrochloride 3.5% gel is placed into the superior cul-de-sac. The upper lid is everted and xylocaine 2% with 1 to 100,000 epinephrine is injected adjacent to the concretion. This is done for local anesthesia and vasoconstriction to reduce bleeding during the procedure. The eye is prepped with one drop of povidone iodine 5% ophthalmic solution, and the face is covered with a sterile fenestrated drape.
Prior to surgery, the site is tested to ensure anesthesia has taken effect. Once this is confirmed, the surgeon makes a horizontal incision through the palpebral conjunctiva above the concretion, then scrapes and removes the concretion with a curette. Next, pressure is applied over the incision with a sterile cotton applicator for hemostasis. After hemostasis is achieved, topical antibiotic ointment is applied for prophylaxis. Cauterization and suturing of the surgical site are not usually necessary. The incisions are small and will stop bleeding with applied pressure and heal by secondary intention (deliberately leaving the wound open, allowing the body to heal on its own).3
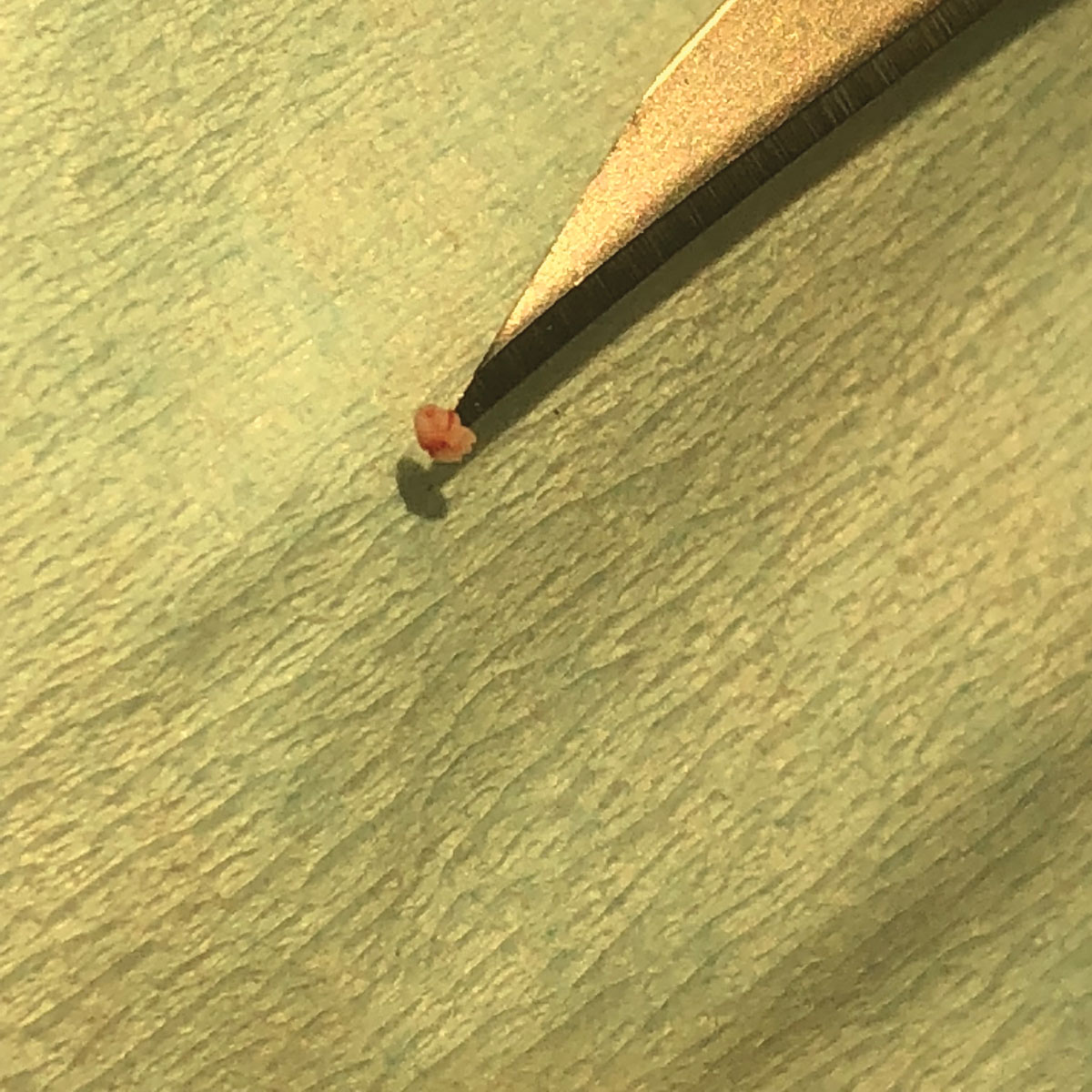 |
| Concretion in curette after excision. |
Post-op Considerations
This procedure is typically well tolerated, and patients will heal in a few days without complications. The eyelid may be tender with slight swelling. Patients are given topical antibiotic ointment with instructions to apply it to the surgical area two times per day for a week. A follow-up appointment is usually unnecessary, although patients should return if they notice discharge, pain, redness, swelling or other signs of infection.
Mrs. Giannonatti is a fourth-year student at Pacific University College of Optometry.
Dr. Skorin is a consultant in the Department of Surgery, Community Division of Ophthalmology in the Mayo Clinic Health System in Albert Lea, MN.
|
1. Bowling B. Kanski’s Clinical Ophthalmology, A Systemic Approach, 8th ed. Philadelphia: Elsevier; 2016:131-66. 2. Mannis M, Holland E. Cornea, 4th ed. Philadelphia: Elsevier; 2017:856-74. 3. Skorin L, Genereux L. Secondary intention healing of graft donor site wound dehiscence following ectropion repair with autologous graft. Clin Surg Ophthalmol. 2014;32(4):101-2. |

