 |
Q:
A 52-year-old Caucasian male presented with unexplained vision loss in both eyes. He’s a 10-diopter myope, which of late has increased by two diopters, and the referring doctor noted an “early” cataract. The patient was sent for a retina consult and possible neuroimaging. Is the answer hiding in plain sight?
A:
This doctor should be commended for raising red flags on vision not correctable to 20/20 without an obvious explanation. “When I get referrals for unexplained vision loss, I initially think about occult corneal irregularity, milky NS, subtle retinal conditions like an epiretinal membrane or lamellar hole, and neurological issues,” says Edward Wasloski, OD, clinical director at Omni Eye Specialists of Baltimore. Once you have ruled out corneal problems with the slit lamp and topography, and retinal problems with a dilated exam and OCT, turn your thoughts to a diagnosis of milky nuclear sclerotic cataract or ‘milky NS,’ says Dr. Wasloski. The majority of the time, taking a thorough history and listening to the patient will lead you to the proper diagnosis. “The first thing I ask about are halos, monocular ghost images, or diplopia,” explains Dr. Wasloski. “Double vision is not something any of us necessarily like to deal with, but when you can demonstrate it in one eye only, the culprit is usually either cornea or cataract.”
 |
| In the absence of posterior and anterior segment findings, think about a diagnosis of “milky NS." |
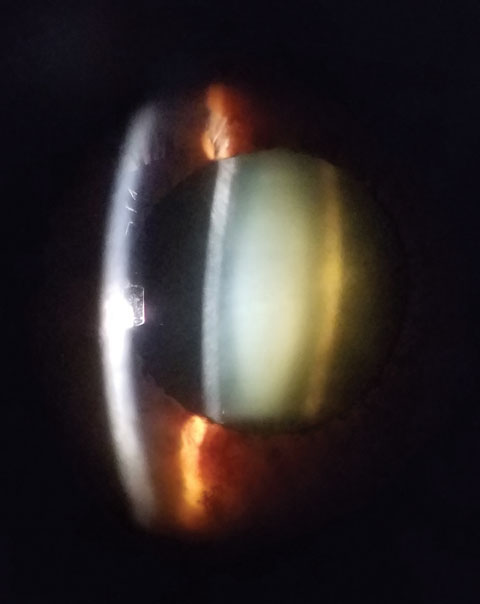
Key characteristics include a central dark reflex on retinoscopy and the characteristic biomicroscopic appearance of a ‘lens within a lens.’ The opalescent or milky white appearance of the nucleus with no surrounding brunescence or cortical spoking is pathognomonic.
Often, a shift in nearsightedness is noted, ranging from one to six diopters. “The patient will also be complaining of significant glare and haloes around lights, especially at night. On dilated exam, note the bowing of the fundus beam that almost appears as if a staphyloma is present wherever the beam is placed on the retina,” says Dr. Wasloski. This is most apparent through the old Hruby lens, rarely used today, but can still be seen to a lesser degree with handheld lenses behind the slit lamp.”
Dr. Wasloski says that the view through these cataracts is often very clear, which is what can throw you off. The more common brunescent or posterior subcapsular cataracts will obscure your view into the eye, which will be consistent with the patient’s view out. “Always think milky NS when the cataract doesn’t look like it can cause the level of acuity reduction that you have measured,” he says. Milky nuclear sclerotic patients are typically younger, with no associated medical conditions or medication use. The cataracts are often asymmetric between eyes.

