 |
Hyaluronic acid (HA) eye drops (i.e., sodium hyaluronate and hyaluronan) are the most commonly used dry eye therapies in Europe and Asia.1 Even our Canadian neighbors have an over-the-counter option with Hylo (sodium hyaluronate, CandorVision). While taking a closer look at a therapy you don’t have may seem frivolous, it makes plenty of sense once you see the various products we can access and the future role of HA in the United States. This successful treatment option might be more accessible than you think.
What’s Special About HA
HA is a high molecular weight naturally occurring polysaccharide known as a gycosaminoglycan. It is found in the human body in connective tissue, synovial fluid and in the aqueous humor and vitreous of the eye.2,3 HA has three primary characteristics that make it useful:
An ability to bind or retain water. HA has a high concentration of hydroxyl groups that result in hydrogen binding.4 Studies show it can bind up to 1,000 times its weight in water, making it highly valuable as a wetting agent.5 The unique structure involves coiled chains that allow water to be trapped within them.6
Viscoelasticity. This allows for shear stress and has been shown to stabilize the tear film and reduce symptoms of DED.7
Wound healing. Research shows HA clinically aids in epithelial cell proliferation, epithelial healing and epithelial migration.8-12 Studies also demonstrate HA’s ability to increase healing of corneal abrasions and alkali chemical injuries in rabbits.13
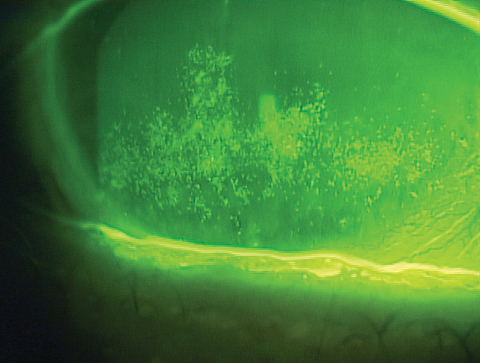 |
| Patients with signs and symptoms of dry eye disease, such as the confluent superficial punctate keratopathy seen here, often benefit from therapies containing hyaluronic acid. |
How You Can Use It
Research shows HA is quite effective in improving the symptoms of dry eye disease (DED), visual functioning in dry eye and even post-surgical patients.14 Thus, manufacturers include it in several products on the market today, and researchers are exploring its effectiveness for any number of therapies:
Artificial tears. Viscosity-enhancing agents are critically important to artificial tear products, and different products use various agents, such as HA, polyacrylic acid, carboxymethyl cellulose, dextran, HP-guar, hydroxypropyl methyl cellulose, polyvinyl alcohol, polyvinylpyrrolidone and polyethylene glycol.15
A key characteristic of a high-quality HA therapy is the molecular weight, which is related to the length of the chain of each molecule. High molecular weight HA will be more cohesive and low molecular weight HA will be more dispersive. Examples of drops containing long-chain HA include Oasis Tears, Oasis Tears PF and Oasis Plus (Oasis Medical).
The concentration of HA does not necessarily reflect the molecular weight, as it is possible to have a high concentration of low molecular weight HA in a formulation.
Research shows Blink Contacts (Johnson & Johnson Vision), which contains 0.15% HA, increases tear break-up time and improves comfort and lens tolerance in contact lens-wearing patients.16,17 Other studies of HA also noted increased tear break-up time for both evaporative and aqueous deficient DED.18
Contact lenses. Although most research focuses on the use of HA in dry eye and corneal wound healing, some studies are specific to contact lens wear. One study of 3 o’clock and 9 o’clock staining in patients wearing rigid gas permeable (RGP) lenses showed a statistical improvement in those treated with 0.1% sodium hyaluronate after two weeks compared with those treated with artificial tears.19 HA can also decrease protein adhesion to contact lenses and can increase hydrophilicity.20
Researchers have also been working on hydrogel contact lenses that can release HA at a controlled rate.21,22 Studies show daily disposable and extended wear contact lenses infused with HA—either by the soaking method or direct entrapment—allow for slow release of HA throughout the day and have proven better wettability and even improved symptoms of dry eye.21,22
The addition of HA to some contact lens solutions such as BioTrue (Bausch + Lomb) could be part of the reason why they work so well for some patients.
Cryopreserve amniotic membrane. New research has also uncovered reasons why cryopreserved amniotic membrane is so effective in corneal wound healing, and one key is long-chain hydrocarbon (HC) HA. In a study that compared cryopreserved with dehydrated amniotic membrane, data shows that cryopreservation better maintains the structural and biological signaling molecules of fetal tissues. The analysis found the HC-HA and pentraxin 3—a protein in the complement pathway of the immune system critical to inflammation treatment—present in cryopreserved formats were absent in the dehydrated tissue.23
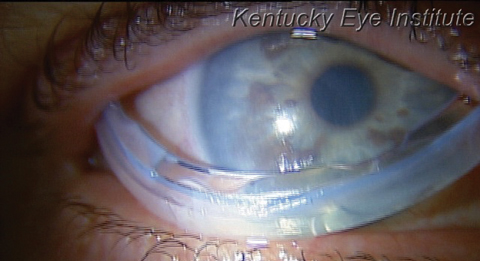 |
| Cryopreserved amniotic membranes, such as the Prokera (Bio-Tissue) seen here mid-insertion, provide HC-HA to the ocular surface and better preserve the structural and biological signaling molecules compared with dehydrated membranes.23 |
Crosslinked HA. Finally, exciting technologies on the horizon for eye care include crosslinked HA. This compound resists degradation and adheres to the ocular surface for extended periods, without blurring.24 A recent study demonstrates that crosslinked HA hydrogel accelerated the time to corneal wound closure compared with a non-crosslinked HA solution in companion animals.25 This investigation involved 30 dogs and 30 cats with spontaneous acute corneal ulcers being treated with either crosslinked HA or a non-crosslinked HA solution (n=15 per group for each species), three times daily until the ulcer healed.25 The investigators then used 25 dogs with persistent non-healing corneal ulcers treated twice daily until the ulcer healed. In all cases the crosslinked HA showed significantly accelerated healing time.25
A poster at the 2017 American Society of Cataract and Refractive Surgery meeting showed how this therapy translated to humans.26 Researchers randomized 39 patients undergoing bilateral photorefractive keratectomy (PRK) with greater than 8mm epithelial defects to three groups: those receiving a crosslinked HA and a bandage contact lens, patients with crosslinked HA alone and those with a bandage lens and artificial tears. The most effective treatment was the crosslinked HA alone with more than 83% of the patients healing within three days compared with an average of 53.8% with today’s current therapy choice of bandage contact lens post-PRK.26]
HA has numerous current applications in eye care, and US optometrists can take advantage of its clinical benefits with some artificial tear products, contact lens solutions and amniotic membrane therapies. Given the promising research on HA, clinicians should hopefully have many more exciting innovations to look forward to in the near future.
Note: Dr. Karpecki is a consultant for many companies mentioned here.
1. Vogel R, Crockett RS, Oden N, et al. Demonstration of efficacy in the treatment of dry eye disease with 0.18% sodium hyaluronate ophthalmic solution (vismed, rejena). Am J Ophthalmol. 2010 Apr;149(4):594-601. |

