 |
History
A 33-year-old white female presented with a chief complaint of blurry vision in her left eye more so than in her right for three months.
She reported that the persistent blur developed after an auto accident. She reported that, during the accident, she hit one side of her head on the back of the passenger seat, in a slow-moving vehicle while not wearing a seat belt.
Her previous ocular and systemic histories were unremarkable and she denied any known allergies to medications or other substances.
 |
| This 33-year-old patient experienced blurred vision three months after an automobile accident in which she sustained head trauma. Can you identify the cause? |
Diagnostic Data
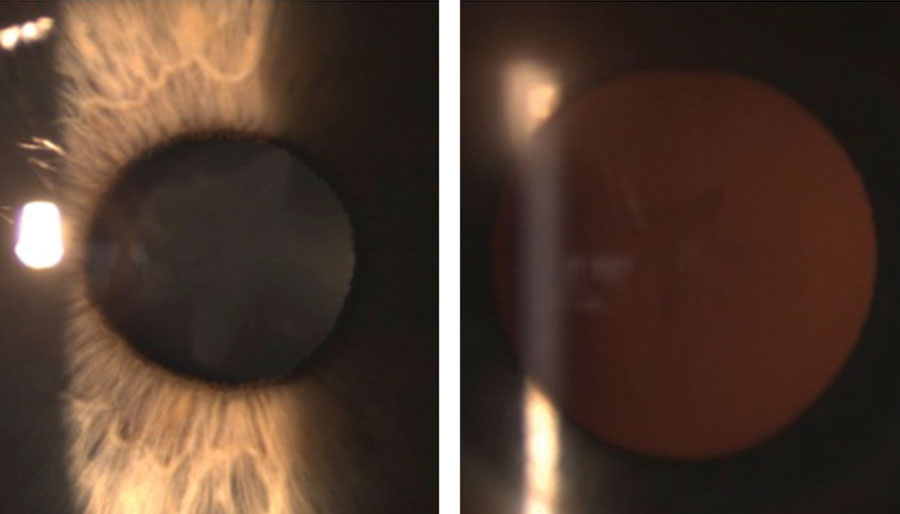
Her best-corrected entering visual acuity was 20/20 OD and 20/30 OS at distance and near. Refraction revealed hyperopia of +0.75D OD and +1.50D OS with no improvement in vision. The pertinent biomicroscopic findings are illustrated in the photographs. Her intraocular pressures were measured at 15mm Hg OD and 18mm Hg OS using Goldmann applanation tonometry.
The patient’s dilated fundus examination revealed no significant posterior pole or peripheral retina findings: the nerves were distinct with cup-to-disc ratios of 0.3/0.35 OD and OS.
Discussion
Additional tests would include laser interferometry to assess macular potential. Optical coherence tomography of the macula could be completed to rule out the presence of vitreomacular traction or the formation of macular hole. A more extensive history should be performed to ascertain the patient’s needs for surgery as well as to understand their expectations.
The diagnosis in this issue is rosette cataract secondary to the blunt trauma to her eye sustained as a result of the auto accident. Trauma remains the leading cause of monocular blindness in patients 45 years old or younger.1-4 Males are affected four times more than females and clinical findings may present as a result of acute, sub-acute, or longstanding sequelae.1
Acute traumatic cataracts, also known as stellate or rosette cataracts, are transient anterior or posterior subcapsular lenticular changes caused from mechanical blunt or penetrating trauma.2-4 They may be stable or progressive and occur due to shearing forces that introduce pathologic changes to lenticular composition.4,5 Courville et al5 introduced the concept of coup (direct force injury) and contracoup (opposite the direct force) to traumatic injury.5 Contracoup injury is based upon secondary shockwaves that transverse the location and axis of impact.5 Resulting contralateral expansion of the lens induces tissue remodeling and accelerated opacification. This mechanism also is what shapes the classic stellate shape of the rosette cataract.5
Initial morphologic changes include intercellular vacuoles within the lens epithelium and the swelling of superficial cortical lens fibers.4 Fiber degeneration within the edematous zone causes fragmentation of fiber cytoplasm into droplets and globules along with the formation of abnormal membrane arrangements and enlargement of intercellular spaces.4 “Rosette” opacities manifest as sharply demarcated layers of vacuolic degeneration in the deeper cortex.4 Dysfunction of the lens epithelium leads to edema of superficial cortical lens fibers that subsequently undergo degeneration and produce a localized lamellar zone of vacuolation.4 This layer becomes compressed and displaced deeper into the cortex.4
Treatment depends on the location of the cataract in relationship with the visual axis.7,8 Prognosis is not only based on the severity of injury itself but also in concert with the significance of adjacent associated ocular injury.1-8 Glaucoma, ocular inflammation, macular edema, retinal detachment, macular hole formation are just some of the co-morbidities.
Standard phacoemulsification can be performed when normal lens capsule integrity and sufficient zonular support is present.7,8 Anytime the stability of the zonules is absent or if the capsule has sustained a rupture in cases such as Marfan’s syndrome, homocystinuria, pseudoexfoliation syndrome the strategy for repair must be altered. Pars plana lensectomy with or without limited vitrectomy is another option.7 The development of synechia, hyphema, inflammation and vitreous hemorrhages can cause surgical solutions to be postponed.
This patient was referred to a surgeon for extraction resulting in an excellent outcome (20/20 uncorrected acuity).
Dr. Gurwood thanks Dr. Luff for contributing this case.
| 1. Puodžiuvienė E, Jokūbauskienė G, Vieversytė M, Asselineau K. A five-year retrospective study of the epidemiological characteristics and visual outcomes of pediatric ocular trauma. BMC Ophthalmol. 2018;18(1):10. 2. Schnaidt AG, Schröder AC, Gatzioufas Z, et al. Delayed loss of vision after hammer and chisel injury. Ophthalmologe. 2009;106(11):1017-21. 3. Wollensak G, Eberwein P, Funk J. Perforation rosette of the lens after Nd:YAG laser iridotomy. Am J Ophthalmol. 1997;123(4):555-7. 4. Wollensak G, Eberwein P, Funk J. Perforation rosette of the lens after Nd:YAG laser iridotomy. Am J Ophthalmol. 1997;123(4):555-7. 5. Courville CB. The mechanism of coup-contrecoup injuries of the brain; a critical review of recent experimental studies in the light of clinical observations. 6. Shah MA, Agrawal R, Teoh R, et al. Pediatric ocular trauma score as a prognostic tool in the management of pediatric traumatic cataracts. Graefes Arch Clin Exp Ophthalmol. 2017;255(5):1027-1036. 7. Resch MD, Balogh A, Sándor GL, et al. Vitrectorhexis in penetrating eye injuries in adults. Eur J Ophthalmol. 2018;10:1120672118804387. |

