Ocular surface foreign bodies are a frequently encountered form of ocular trauma, which account for roughly 40% of all ocular traumas and are responsible for nearly 2% of all emergency room visits.1 Patients generally present to the clinic with a very clear history of being struck in the eye with foreign material, but occasionally they have no history other than recent- onset irritation. The material may be metallic, glass, stone or organic and, to some degree, the type should help determine the treatment course. Though patients often have severe discomfort, the level of morbidity seen as a result of foreign body injury is typically mild.
While the actual diagnosis of a corneal foreign body is generally easy to arrive at, the treatment of these injuries warrants more than a kneejerk response. As with any injury to the eye, diagnostic and therapeutic considerations with corneal foreign bodies should include diagnosing the precise nature of the injury, assessing your ability to treat the injury in the acute phase without worsening the course and, given the nature of the foreign body, anticipating and treating any long-term sequelae.
 |
| This patient was referred in for evaluation of scar caused by a foreign body and rust ring removal. Click image to enlarge. |
Identifying the Culprit(s)
Prior to simply removing the offending agent, it’s important to carefully assess the overall status of the eye, the nature of the foreign body and the depth of the injury. Patient- and material-specific features have the potential to increase the risk of complications and should shape the short- and long-term treatment course.
It’s easy to get swept away in the emotion of identifying a problem and offering a treatment; however, before a foreign body is removed and the case is closed, the involved eye needs to be carefully assessed to ensure no secondary ocular surface foreign bodies exist and that there are no signs of a retained intraocular foreign body. Clinicians should carefully assess the anterior segment and scrutinize the cornea, as well as the bulbar and palpebral conjunctiva with and without fluorescein dye—which will highlight areas of epithelial disruption. Corneal assessment should rule out any subtle full-thickness lacerations (which, in the case of small foreign bodies, may be self-sealing due to the heat of a penetrating injury). Iris and pupillary abnormalities, even a subtly peaked iris, also indicate a possible retained intraocular foreign body and should prompt gonioscopy (after foreign bodies have been removed and the globe is relatively patent with a formed anterior chamber and normal intraocular pressure).
Although the anterior chamber will often have a subtle traumatic iritis, if this iritis remains chronic after the material is removed, this is a strong indicator for retained intraocular material, prompting closer examination. Any disruption to the lens or capsule will result in near immediate and significant cataract development, also indicating intraocular penetration and guiding evaluation. If these indicators of intraocular material exist, the patient should be dilated at the initial visit.
The clinician also needs to be aware of the patient’s previous ophthalmic history. Previous corneal surgery, particularly LASIK, can impact prognosis when dealing with a foreign body that has penetrated into the flap interface. Issues with epithelial ingrowth may develop in this scenario. Keratoplasty patients also need to be flagged, as rupture of the interface could occur with aggressive removal, particularly in relatively fresh transplants. These patients are at a greater risk for drug-resistant superinfections.
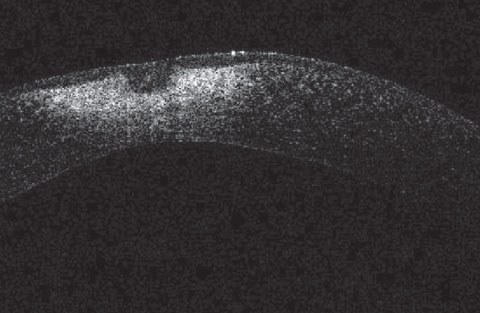 |
| This corneal OCT of the patient from first image shows significant corneal scarring too deep for PTK. This case highlights how aggressive use of an Alger brush for rust removal can lead to significant corneal scarring. |
Nature of the Foreign Body
The foreign body’s makeup is most typically related to the specific history at the time of the injury. Welding and grinding histories will produce metallic foreign bodies, striking tools will produce stone/ceramic or metallic objects and landscaping injuries (often caused by string trimmers) will involve organic or stone material (though the stone material in these cases should be treated similar to organic material, as it pertains to infection risk).
Finally, pet tarantulas, while infrequently encountered, are a well-described source of ocular surface foreign bodies, as their leg hairs may periodically end up on the ocular surface when a patient who had recently handled their pet rubbed their eyes. These fibers are barbed and can embed themselves readily into the cornea as well as the conjunctiva.
As with any foreign body, primary material considerations include the formation of corneal rust with metallic ferrous material, risk of infection with organic material or risk of contamination with fungal material or atypical bacteria species when the material is from an unclear environmental source.
Clinicians should carefully assess the depth of the foreign body prior to removal, as deep glass, ceramic or stone need not be removed if it doesn’t impact vision, and very deep metallic or organic material should likely be referred to a specialist due to risk of penetration and advanced scarring.
Though it may seem simple to assess depth, in many cases it can be difficult to clearly demarcate the level of penetration; thus, close examination with a thin optic section is warranted. In unclear cases, corneal OCT can clearly demonstrate zones of penetration.
The depth of the injury should also be considered prior to using an Alger brush burr on corneal rust rings. Alger brush burrs are widely reported as having a pressure-sensitive clutch that will prevent the mechanism from penetrating Bowman’s membrane; however, if the foreign body itself is penetrating Bowman’s membrane, there is no longer an effective resistance to initiate the stop, which can lead to wide scarring if used aggressively.
In cases of penetrating injuries, you should stabilize the globe and then refer for specialist evaluation.
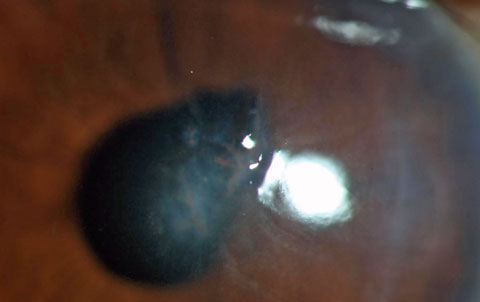 |
| Deep stromal retained foreign body from a string weed trimmer. Note the distortion of the pupil, indicating the injury was penetrating and highlighting the potential for a retained intraocular foreign body. Given the nature of the injury, there is a significant risk for microbial keratitis or endophthalmitis. |
The Acute Injury
Barring a penetrating or inert/deep foreign body, the material should be removed with the patient under topical anesthesia in the clinic. With good patient cooperation, this is possible without a lid speculum, but when blepharospasm is intense, clinicians should use a speculum. In very superficial cases, the material may often just be wiped away with a cotton-tipped applicator. In deeper cases, more invasive means are necessary.
Depending on clinician preference, there are a number of acceptable devices for removal of a corneal foreign body: golf spud, jeweler’s forceps, magnetic probe or small- gauge needles. All instruments should be sterile. The goal is total removal of the material and any small particles left behind after removal of the primary foreign body. However, stromal disruption will lead to scarring, and broad disruptions here should be limited when not necessary.
Any foreign body containing iron will cause rust deposition to the adjacent cornea shortly after contacting the ocular surface. The mechanism probably involves the immune response to a ferrous foreign body as opposed to simple inoculation and diffusion, and is not related to the thermal status of the foreign body.2
Regardless of the precise physiologic origin of corneal rust rings, their presence will often induce inflammation and slow down healing and result in localized stromal necrosis, as opposed to the numerous other forms of iron deposits that occur within the cornea such as Hudson-Stahli lines, Stocker lines and Fleicher rings. These should generally be removed as thoroughly as possible when encountered.3,4 As with removal of the foreign body itself, rust ring removal can be accomplished with several different devices, most popular among these being a small-gauge needle and an ophthalmic burr. Clinical studies show more even and complete removal of the rust with burr compared with manual removal with a needle, and also facilitates more rapid healing; however, one animal model of rust ring removal showed a tendency for deeper scarring when the burr was used.1,5 Again, though removal of corneal rust will help facilitate a rapid healing response, widespread stromal application of the burr can lead to significant scarring. Removal of all rust material over several visits, as more peripheral rust material may migrate superficially, may be preferable when the ring is large and deep and some material isn’t easily removed. During this period, rust that doesn’t stymie corneal healing can be left in place.6
Once removal of the foreign body and any rust ring has been accomplished, the patient should be treated in a similar fashion as patients with a corneal abrasion. Topical antibiotics should be applied in all cases. While generic ophthalmic antimicrobials are acceptable in cases without concerning history, in those with a concerning history a newer generation fluoroquinolone should be prescribed. In these cases, I generally prefer Vigamox (moxifloxacin 0.5%, Alcon) due to its lack of preservative. Though clinicians should be aware of the risk for fungal infection and extend follow-up intervals and total follow-up course in the setting of high-risk foreign bodies, treatment with a prophylactic antifungal is not warranted in most cases.
For comfort, cycloplegia can be helpful and limited dosing with topical ophthalmic NSAIDs may also reduce pain, though these drops may occasionally lead to corneal healing issues. A bandage contact lens may also be used until closure of the epithelial defect. More advanced therapy with amniotic tissue could be used but is not necessary in most cases. A corticosteroid (alone or as a combination antibiotic topical steroid) should generally not be used in cases of organic corneal foreign body (even with traumatic iritis) until epithelium has healed due to the risk of potentiating severe infection. In cases where scarring that limits vision is a concern, amniotic tissue may be applied, as it may help mitigate superficial scarring risk to some degree. Follow-up should occur shortly after to ensure appropriate healing and allow for removal of a bandage soft contact lens when used.
Post-Trauma Considerations
Follow-up considerations of corneal foreign bodies should also involve treatment of any sequelae that may arise. To allow timely diagnosis of complications, in addition to follow-up one to two days after injury, clinicians should follow up approximately a week later, though these recommendations may vary on a case by case basis. Problems that develop days and months following the original injury could be as mundane as a poorly healing eye or as significant as microbial keratitis. Occasionally, a foreign body and its removal may leave a visually significant scar, which should be assessed for its ability to be removed.
 |
| Plant seed corneal foreign body carries increased risk of microbial fungal keratitis. Click image to enlarge. |
What Can Go Wrong?
Sometimes, patients with foreign body removal present upon follow up with complications, such as:
Non-healing wound. In almost all cases, epithelial defects from corneal foreign bodies heal quickly and without complication once the foreign body and any rust ring has been removed. Non-healing most typically occurs when a corneal rust deposit is not sufficiently removed, and results in an area of necrosis. At this point, an Alger brush or small-gauge needle will often more easily remove the residual corneal rust compared with the initial visit. Any necrotic tissue, which also retards epithelialization, should also be debrided. If you aren’t sure whether you are dealing with necrotic tissue or an infiltrate, which can look similar (though behave quite differently when mechanically debrided—necrotic tissue is generally softer and more easily debrided than an infiltrate), culturing the material on a prepackaged swab would be appropriate. In cases where there is no necrosis or remaining corneal rust, neurotrophy, exposure or severe ocular surface disease could be the culprit, as each of these can slow healing and should be carefully assessed and treated. Although they aren’t necessary in most cases of corneal foreign bodies, in any non-healing corneal defect, a sutureless amniotic membrane is a great option to speed things up. Continuing antibiotic therapy at effective dosages is necessary as long as an epithelial defect persists.
Infection. Non-surgical trauma of the ocular surface is the greatest risk factor for infectious keratitis in developing countries and is also responsible for a significant proportion of cases in the United States. Fungal infection carries a well-known association with corneal trauma from plant matter, but other infectious etiologies, such as non-tuberculous mycobacteria, Nocardia and Acanthameoba all are distributed widely throughout the environment and are associated with external trauma. Foreign body injuries from suspicious sources should be followed closely for a longer period and should likely be treated with stronger antibiotics than those from cleaner material. Infiltrates that develop from sites of external traumas need to be cultured and treated aggressively, or referred to a specialist, as in many of these cases you are dealing with an atypical organism.
Recurrent corneal erosion (RCE). This is a frequently encountered clinical entity that is often associated with trauma, in most cases a superficial laceration of the corneal epithelium and Bowman’s membrane by a fingernail. Given the shared traumatic etiology, a corneal foreign body injury may seem like a likely source for RCE to develop from. The reality, however, is that foreign bodies rarely cause this condition. The rationale for this difference has to do with depth of injury and the pathophysiology of RCE. Any injury that removes epithelium but doesn’t impact Bowman’s membrane will heal uneventfully. Any injury that removes epithelium and irregularly disrupts Bowman’s membrane but doesn’t disrupt the stroma has a greater chance for leading to RCE, as the epithelial anchoring complexes are disrupted in these cases. However, any injury that irregularly disrupts the epithelium, Bowman’s membrane and stroma has a low rate of RCE because of the scarring associated with activation of keratocytes (which occurs in cases of stromal trauma). This leads to strengthening of the epithelial-stroma adhesion and a low risk of RCE. In most cases, corneal foreign bodies penetrate through to the stroma, so there is very little association with RCE.
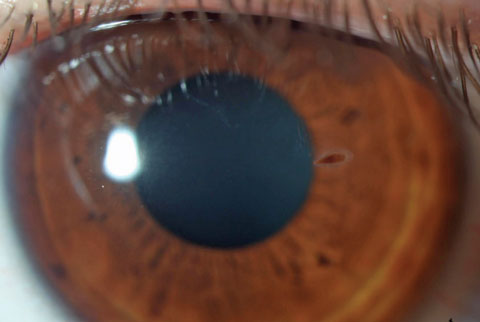
 |
| A small piece of retained glass is present in the mid stroma. The material is out of the visual axis and inert and so can be left alone. |
Post-traumatic Scars
Scarring occurs in all cases of stromal injury and some degree of it should be expected after foreign body removal. In many cases of small focal injury, this scarring doesn’t impact vision to any significant degree, even when the visual axis is involved. Occasionally, however, with a large, widespread (such as occurs from shattered glass) or deep foreign body injury, stromal scarring may be significant and resultant disruption to vision may occur. In these cases, surgical options may be considered. For any surgery, it is best to have the patient wait a minimum of six months following the injury to allow the eye to heal completely. If vision or keratometric measures change significantly over this period, the patient should wait another six months; for any surgical fix it’s important to have a relatively stable cornea. Once the cornea stabilizes, surgical options to consider include: corneal transplant; penetrating keratoplasty (PK) or deep anterior lamellar keratoplasty (DALK) for deep central corneal scars; or phototherapeutic keratectomy (PTK) for anterior stromal scarring.
While transplant for a foreign body scar is uncommon, PTK is frequently used in this capacity. PTK uses the excimer laser to remove corneal tissue and can quite effectively treat superficial opacity or even zones of irregular corneal astigmatism, both frequently encountered sources of vision loss from corneal scars. In most cases, as with traditional PRK, the surgery center won’t remove tissue beyond a residual stromal bed of 300µm to 350µm and so the scars need to be anterior. Further, as the procedure results in removal of corneal tissue, a flattening effect occurs, which reduces myopia or increases hyperopia, a feature that can be useful in some cases and a drawback in others. Antihyperopia treatments can be used when this shift is not desirable, but hyperopic laser treatments aren’t as accurate or effective long-term as myopic treatments.
It should also be noted that any excimer application for irregular astigmatism secondary to a scar has less precise outcomes and appropriate patient counseling about the goal of the procedure (reducing, but perhaps not eliminating, irregularity) is crucial. As part of the workup for these patients, a diagnostic rigid gas permeable (RGP) spherocylinder over-refraction can be useful to determine the amount of reduced vision from corneal irregularity (which the RGP will correct) or opacity (which the RGP will not correct) and can help guide surgical decision-making.
For deep or full-thickness scars, PK and DALK may be options to consider. Given the expense of the surgery, length of recovery, risk of complication and uncertain refractive endpoint, PK and DALK should be reserved for visually significant scars that cannot be correct with an RGP.
Given the frequency with which corneal foreign body injuries occur, most ODs are well-versed in their management, though if you are not used to performing manual manipulations to the eye, or haven’t dealt with one of these cases in time, some subtler aspects of their care can be overlooked. As with the management of any acute ocular injury, it’s important to be mindful of both acute considerations (material, depth, degree of compromise to ocular tissue) and chronic considerations (potential for scarring, infection and poor healing) prior to initiating treatment to ensure best outcomes and appropriate patient expectations.
Dr. Bronner is an attending optometrist at Pacific Cataract Laser Institute in Kennewick, Wash.
|
1. Bowes Hamill M. Mechanical Injury. In: Krachmer JH, Mannis MJ, Holland EJ. eds. Cornea. 2nd ed. St. Louis: Mosby;2004:749-76. 2. Dilly N. What is a Rust Ring. Cornea. 2012;31:1355-7 3. Jauamanne DGR, Bell RWD. Non-penetrating corneal foreign body injuries: factors affecting delay in rehabilitation of patients. Journal of Accident and Emergency Medicine. 1994;11:195-7. 4. Brown N, Clemett R, Grey R. Corneal rust removal by electric drill. Br J Ophthalmol. 1975;59: 586-9. 5. Sigurdsson H, Hanna I, Lockwood AJ, Longstaff S. Removal of Rust Rings, Comparing Electric Drill and Hypodermic Needle. Eye. 1987;1:430-2. 6. Liston RL, Olson RJ, Mamalis N. A comparison of rust-ring removal methods in a rabbit model: small-gauge hypodermic needle versus electric drill. Annals of Ophthalmology. 1991;23:24-7. 7. Rapuano C, Luchs JI, Kim T. Anterior Segment Trauma. In: Anterior Segment; The Requisites in Ophthalmology. Mosby;2000:115-118. |

