 |
Q:
I have a Sjögren’s disease patient with a dry eye flare up and complications. No topical treatments have helped. What’s next?
A:
“I saw this patient for irritation and burning in both eyes about a year ago,” says Brian Den Beste, OD, of LASIK Pro Eye Consultants in Orlando. The patient, a 62-year-old Caucasian female who Dr. Den Beste had seen on and off for significant dry eye and narrow angles, had a long-standing history of Sjögren’s disease and chronic fatigue syndrome.
At the time of the aforementioned visit, the patient had stopped wearing her soft contact lenses based on instructions from her primary care optometrist, but was using artificial tears 10 times a day. “I suggested a mild steroid and added oral doxycycline, as she demonstrated mild facial rosacea and chronic lid margin changes characteristic of posterior blepharitis,” says Dr. Den Beste. “I thought her complaints were more inflammatory in nature rather than arising from a lack of tears.”
When she returned a week later with a 3mm oval abrasion above fixation in the right eye, Dr. Den Beste stopped the steroids and placed a bandage soft lens on the eye. After a two-week period of follow-up and several different bandage lenses, not much had changed. Instead, Dr. Den Beste tried a Prokera (Bio-Tissue) amniotic graft. While the abrasion shrunk significantly over the next five days, the surrounding epithelium began to show intense staining.
At this point, Dr. Den Beste went with a bland ointment and autologous drops formulated from a 50% concentration. After using the combination every two hours for a period of three weeks in both eyes, the patient felt much better, initially. “Her punctate changes were much improved and she was much more comfortable,” says Dr. Den Beste.
A week later, however, the patient came back with a large abrasion on the inferior cornea of her right eye. “The surrounding anterior stroma demonstrated white blood cell migration, so I prescribed a topical fluoroquinolone,” says Dr. Den Beste. Again the patient’s infiltrate resolved and she went home with a bandage lens. One more week later, though, she came back with yet another large epithelial abrasion. Also, her previous inferior lesion showed stromal thinning. “After four months of steroids, bland ointment, autologous drops, amniotic membranes, moisture chamber goggles and bandage contacts, I sent her to her rheumatologist and suggested she be given a biologic response modifier or a traditional disease-modifying antirheumatic drug (DMARD),” says Dr. Den Beste.
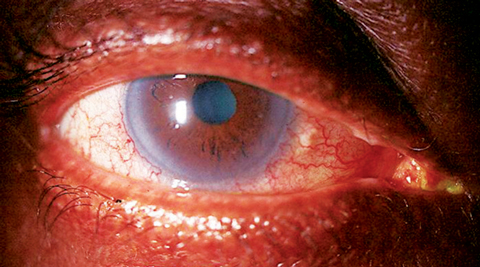 |
| Sjögren’s patients often present with inflammatory dry eye, shown here. Photo: Alan G. Kabat, OD |
The Fix
Per Dr. Den Beste’s request, the rheumatologist gave the patient 200mg of Plaquenil (hydroxychloroquine, Sanofi-Aventis). Within two weeks, her condition changed dramatically; the abrasions resolved and her comfort returned. “Plaquenil is an older DMARD but it is still used, especially for patients with lupus,” says Dr. Den Beste. “It is not clear how the drug works, but it is thought to block pro-inflammatory pathways.” According to Dr. Den Beste, large sterile ulcers that occur in the periphery can lead to extreme corneal thinning and perforations, typically in patients already on medications for serious autoimmune conditions, such as Sjögren’s.
“This case was unusual, however, because the patient was under the care of a rheumatologist and was thought to be doing fine systemically,” says Dr. Den Beste. “It wasn’t until she broke down from an ophthalmic standpoint that we recognized she needed oral medication for her rheumatologic disease.”
According to Dr. Den Beste, corneal involvement in patients with severe autoimmune diseases such as rheumatoid arthritis can typically be managed with topical medications and, occasionally, oral steroids. However, sometimes they require ongoing treatment with a DMARD or a biologic response modifier such as Humira (adalimumab, AbbVie).
“As ODs, we often call on rheumatologists when dealing with severe uveitis or scleritis,” says Dr. Den Beste. “The lesson here is to consider that same referral when dealing with recalcitrant dry eye and corneal inflammation.”

