Stress and AMD: Recognize the Link
New research suggests ODs should be looking at more than a patient’s visual acuity and ocular anatomy.By Rebecca Hepp, Managing Editor
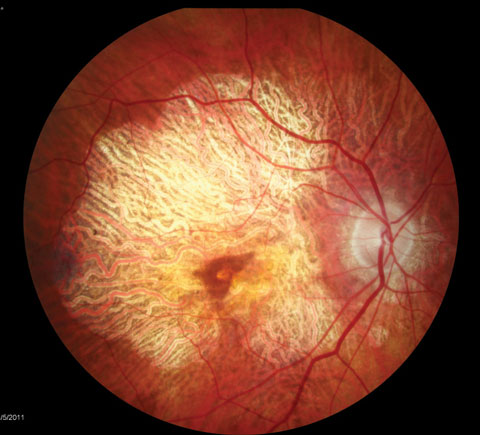 |
| AMD patients require education about influences on their ocular status, and that includes stress. Photo: Julie Poteet, OD |
The researchers used the Perceived Stress Scale (PSS) with 137 patients with AMD and found it is a useful method of evaluating the connection between patient stress and vision loss associated with AMD. Using Rasch analysis to discover how well the PSS measured perceived stress, the study authors found nine of the 10 questions commonly used for the PSS performed well with the study participants and were able to differentiate between patients with higher vs. lower levels of perceived stress.
“Understanding a patient’s level of perceived stress could help identify those who would benefit from interventions for managing stress,” says Bradley E. Dougherty, OD, PhD, assistant professor at the Ohio State University College of Optometry and study author. “While it may not be commonly considered, as it’s not directly related to the eye, the identification and management of perceived stress should be thought of as important to the complete care of the patient. Stress has a negative effect on patients’ overall quality of life.”
According to the authors, AMD patients are known for their increased rates of psychological symptoms. In addition, previous research shows PSS scores are related to increased cortisol levels, susceptibility to infection, increased proinflammatory cytokines and slow wound healing, to name just a few negative health outcomes.
“A first step optometrists could take is using a survey such as the Perceived Stress Scale to formally evaluate perceived stress levels,” Dr. Dougherty says. “From there, optometrists could familiarize themselves with local mental health providers and with other strategies that could be effective for patients to manage their own stress.”
The authors also note previous research found perceived stress as measured by the PSS can be predictive of inflammation—and AMD is an inflammatory disease. “We are investigating the relationships among stress and things such as visual acuity, change in vision with treatment and self-reported visual function,” Dr. Dougherty says.
“We are also interested in determining whether the increased inflammation that can result from high levels of stress may negatively affect AMD treatment results. To accomplish this, we are measuring C-reactive protein levels, which are known to be associated with AMD incidence, and investigating how those might be related to treatment outcomes.”As research digs deeper into the relationship between stress and disease progression, clinicians can treat the whole patient now, and the PSS is a good tool to start with, the study concluded.
| Dougherty BE, Cooley SL, Davidorf FH. Measurement of perceived stress in age-related macular degeneration. Optom Vis Sci. 2017;94(3):290-6. |
Old Drug Shows Promise for Retinal Disease
The breast cancer drug tamoxifen appears to protect against photoreceptor degeneration, according scientists at the National Eye Institute (NEI).
The drug prevented immune cells from removing injured photoreceptors in an animal model of retinal injury, suggesting tamoxifen might work for treating age-related macular degeneration (AMD) and retinitis pigmentosa (RP).1,2
While using tamoxifen in the laboratory to activate specific genes in mouse models, researchers observed that mice treated with tamoxifen gained resistance to light-induced eye injuries and experienced little to no photoreceptor degeneration.1
The team then investigated the effects of tamoxifen on light-induced photoreceptor degeneration in normal mice and mice with a disease similar to RP.2 Results showed significantly lower levels of photoreceptor degeneration compared with control mice that did not received tamoxifen. Tamoxifen-treated mice also demonstrated higher photoreceptor function, compared with controls, according to the study.1,2
“What’s interesting is that tamoxifen, a medication linked to retinal toxicity, is now being studied as a neuroprotective drug for the retina in certain degenerative eye diseases,” says Steven Ferrrucci, OD, Chief of the Optometry Department at the VA Sepulveda Ambulatory Care Center and professor at the Southern California College of Optometry at Marshall B. Ketchum University. Reported ocular toxic reactions consist of crystalline retinopathy, corneal deposits and optic neuritis, according to Dr. Ferrucci. The reported incidence of toxic reactions to tamoxifen in the literature varies between 0.9% and 12%.3,4 “For instance, UK researchers looked prospectively at 65 women receiving the standard dose of tamoxifen, 20mg/d, finding that eight patients (12%) developed some form of ocular toxic reaction, while another study found a 3.1% rate of crystalline retinopathy in patients receiving a similar dose,” says Dr. Ferrucci.3,4
In this case, it may be useful in certain diseases such as AMD and RP, says Dr. Ferrucci. “Certainly while exciting news, further investigation in both animal and human studies is needed before we can conclude this is a viable treatment option for such diseases.”
Since the drug dosage in the animal study was equivalent to eight times the FDA-approved dose for breast cancer, the NEI scientists are currently investigating whether lower tamoxifen concentrations garner the same protective benefit.1
The authors say this research forms the foundation for clinical trials, which are not far off, given the established safety of the drug.1
| 1. Breast cancer drug dampens immune response, protecting light-sensing cells of the eye. National Eye Institute. http://nei.nih.gov/news/briefs/breast-cancer-drug-dampens-immune-response-protecting-light-sensing-cells-eye. Accessed March 23, 2017. 2. Wang X, Zhao L, Zhang Y. Tamoxifen provides structural and functional rescue in murine models of photoreceptor degeneration. Journal of Neuroscience. 2017;37(12):3294-310. 3. Alwitry A, Gardner I. Tamoxifen maculopathy. Arch Ophthalmol. 2002;120(10):1402. 4. Lazzaroni F, Scorolli L, Pizzoleo CF. Tamoxifen retinopathy: does it really exist? Graefes Arch Clin Exp Ophthalmol. 1998 Sep;236(9):669-73. |
Legislative Update: FL and GA in Play
Optometrists in Florida are backing a bill that would expand their scope of practice to include some laser procedures. HB 1037, if passed, would allow certified optometrists in ophthalmic surgery to perform laser and non-laser ophthalmic surgery. To become a certified optometrist in ophthalmic surgery, clinicians would have to successfully complete a course and subsequent examination, approved by the board of optometry, on laser and non-laser ophthalmic surgery. The bill passed the House Health Quality Subcommittee and was under review by the Health and Human Services Committee as of March 20.
Injections in Georgia
Georgia optometrists are waging another legislative battle, this time for the right to perform injections. Senate bill 221 would allow optometrists to administer pharmaceutical agents related to the diagnosis or treatment of diseases and conditions of the eye and adnexa by injection, so long as they complete an injectables training program or are enrolled in a program and under an ophthalmologist’s supervision. Despite pushback from Georgia ophthalmologists, the bill passed the Senate 34 to 17 on March 3 and is now under review in the House.
Stem Cells: Handle with Care
A recent study reveals a new stem cell identification method that may eventually allow doctors to restore vision to patients with damaged corneas. Using a technique that involves highly sensitive atomic force microscopy, researchers put pressure on certain cells to better understand their ability to transform into mature cells.1
The researchers were able to differentiate limbal cells as softer and more flexible than other cells studied. Because of this, the new method shows potential as a quick identification system to find transplantable cells in a patient’s own tissue. Researchers also developed a new microfluidic cell-sorting device that could speed up the existing cell sorting process.
“Studies are on track to show that this could be a very helpful procedure, but we’re not there yet,” says James Thimons, OD, an adjunct clinical professor at Salus University.
The Dark Side of Research
Despite these promising advances, a report recently published in the New England Journal of Medicine (NEJM) highlights the potential dangers of stem cell therapy if not handled properly. The report details three women who lost sight after undergoing stem cell treatment for macular degeneration at a Florida clinic. Clinic staff extracted stem cells from the patients’ own belly fat to inject into the eyes, according to a New York Times article.2
Clinicians not associated with the Florida clinic found the patients’ entering acuities ranged from 20/30 to 20/200; one year after the injections, the patients’ visual acuities ranged from 20/200 to no light perception, the NEJM article found.3
To Dr. Thimons, what is most concerning about the report is that both eyes of the patients were operated on in the same day, which is atypical in clinical trials; even many routine surgical procedures are not performed bilaterally same-day.
These cases highlight the significant risk clinics touting the restorative benefits of unproven stem cell therapy pose to the population, as well as to future stem cell research. “You’d hate to see stem cells as a technology placed into a negative public view,” says Dr. Thimons. “It doesn’t take a great leap of faith to believe that a negative headline like this could impact the future of legitimate studies.”
To prevent such issues, he stresses the importance of patient-clinician communication when a patient is looking into clinical trial options, especially those found online.
The Stem Cell Promise
Still, stem cell research appears to be heading in the right direction. The newest research that has allowed investigators to not only identify transplantable cells but also sort them quickly holds huge promise for the future—and clinicians shouldn’t let negative reports of mishandled therapies stymie enthusiasm. “My hope is that we will look at this as a profession and understand the potential of stem cells, and that incidents like these are isolated,” says Dr. Thimons.
|
In the News
North Carolina Senator Danny Britt recently introduced a bill requesting $2.1 million for the creation of a new school of optometry at the University of North Carolina at Pembroke. With no other schools of optometry in the state (the closest being the University of Alabama at Birmingham School of Optometry), Sen. Britt believes the legislative environment is favorable for such a project, and his district would benefit from the new school, according to a press release.
Researchers recently discovered that using SD-OCT to noninvasively measure the peripapillary retinal structure may be a better way to measure intracranial pressure in children. SD-OCT parameters outperformed other conventional clinical measures, suggesting it is an effective surrogate for invasive techniques currently employed. Detecting elevated intracranial pressure in children helps ensure timely intervention and prevent neurocognitive impairment, the study said.
Swanson JW, Aleman TS, Xu W. Evaluation of optical coherence tomography to detect elevated intracranial pressure in children. JAMA Ophthalmol. February 23, 2017. [Epub].
New research suggests larger eyes and better eyesight in air vs. water were key to life’s transition from ocean to land, and even consciousness, according to a recent study. Eyes tripled in size and shifted from the sides to the top of the head long before fish modified their fins into limbs, researchers found. The combination of the increase in eye size and vision through air would have conferred a one million-fold increase in the amount of space within which objects could be seen, according to the researchers.
Maclver MA, Schmitz L, Mugan U, et al. Massive increase in visual range preceded the origin of terrestrial vertebrates. PNAS. March 7, 2017. [Epub].

