 |
History
A 68-year-old female presented to the clinic for an ocular health check with a chief complaint of difficulty reading. Her ocular history was noncontributory. Her systemic history was remarkable for hypertension, for which she was compliant and properly medicated. She had no known allergies.
Diagnostic Data
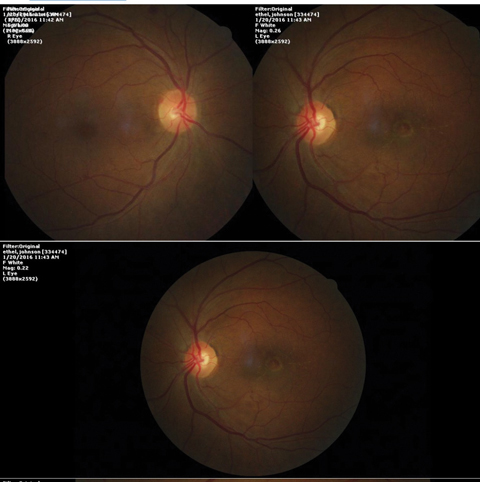
Her best uncorrected visual acuities were measured at 20/25 OD and 20/50 OS at distance and near. Her external examination was within normal limits and there was no afferent pupillary defect. The refraction was negligibly different. Biomicroscopy found normal and healthy anterior segments with evidence of grade II+ nuclear cataracts. Goldmann intraocular pressures measured 14mm Hg OU. The pertinent dilated fundus findings are illustrated in the photograph and the optical coherence tomography (OCT).
Your Diagnosis
Does the case presented require any additional tests, history or information? What steps would you take to manage this patient? Based on the information provided, what would be your diagnosis? What do you believe is the patient’s most likely prognosis?
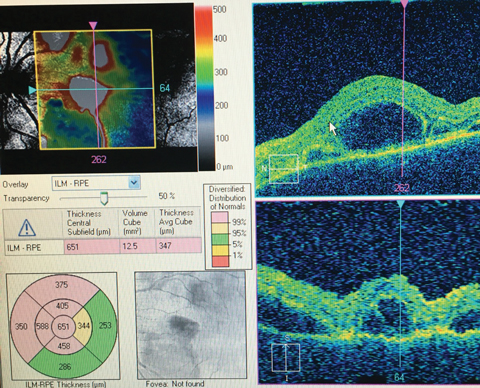 |
| The above OCT readout and the fundus images below show a 68-year-old female patient who presented with trouble reading. Does anything on these images help to pinpoint her diagnosis? |
 |
Diagnosis
Additional testing included additional history regarding systemic health maintenance and baseline fundus photographs. The patient’s vision was checked using the pinhole and laser interferometry. Brightness comparison and red saturation were also tested.
The diagnosis in this issue is neurosensory retinal detachment secondary to age related macular degeneration (AMD), most likely idiopathic polypoidal choroidal vasculopathy or posterior uveal bleeding syndrome. Idiopathic polypoidal choroidal vasculopathy (IPCV) was first identified between 1982 and 1985 as a peculiar hemorrhagic disorder of the macula, characterized by recurrent sub-retinal and sub-retinal pigment epithelium bleeding in middle-aged Black women.1,3,4 The specific lesions are characterized by chronic, multiple, recurrent serous or hemorrhagic detachments of the retinal pigment epithelium (RPE) and neurosensory retina.5 The pathophysiology behind the primary abnormality finds faulty choroidal circulation inducing characteristic lesions of the inner choroidal vascular network producing aneurysmal bulges and outward projecting vessels visible clinically as reddish orange, spheroid, polyp-like structures or as dome like lesion resembling a macular serous detachment.3
The majority of IPCV cases are diagnosed in patients of African and Asian descent.1-4 These patients exhibit signs and symptoms similar to age related macular degeneration.1-3 In Caucasian patients, PCV counts for less than 10% of dry cases and up to 85% of patients with hemorrhagic or exudative retinal pigment epithelial detachment.1 This form of neovascularization has been documented to occur in white patients with or without concomitant drusen with the site of potemtial involvement extended from the peripapillary area to the peripheral fundus.4 Even with the newer optical coherence tomography (OCT), intravenous sodium fluorescein angiography (IVFA) and indocyanine green angiography (ICG) remain indispensable tools for confirming the diagnosis.1,2,4 Although the polypoidal choroidal vasculopathy and AMD share common signs, symptoms and genetic factors, polypoidal choroidal vasculopathy’s clinical characteristics including the way in which it responds to photodynamic therapy, suggests that it deserves recognition as a separate clinical entity.2
Treatment must be considered in active disease threatening the macula.1,2 Combination photodynamic therapy with for closure of PCV complexes and anti-VEGF injection is emerging as the treatment with the highest potential to reduce associated macular edema, limit recurrences and restore vison.1-6
| 1. Coppens G, Spielberg L, Leys A. Polypoidal choroidal vasculopathy, diagnosis and management. Bull Soc Belge Ophtalmol. 2011;(317):39-44. 2. Gomi F, Tano Y. Polypoidal choroidal vasculopathy and treatments. Curr Opin Ophthalmol. 2008;19(3):208-12. 3. Ciardella AP, Donsoff IM, Huang SJ, et al. Polypoidal choroidal vasculopathy. Surv Ophthalmol. 2004;49(1):25-37. 4. Imamura Y, Engelbert M, Iida T, et al. Polypoidal choroidal vasculopathy: a review. Surv Ophthalmol. 2010;55(6):501-15. 5. de Crecchio G, Chan RV, Manzi G, et al. Polypoidal choroidal vasculopathy: recent advances in therapy. Curr Drug Targets. 2011;12(2):206-11. 6. Sato T, Kishi S, Matsumoto H, et al. Combined photodynamic therapy with verteporfin and intravitreal bevacizumab for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2010;149(6):947-954. |

