For more than two decades, laser-assisted in situ keratomileusis (LASIK) has dominated the field of keratorefractive surgery with widespread acceptance as a procedure with high patient satisfaction, high precision and a good safety profile. Within the last few years, however, a new corneal refractive surgery has been making waves: small incision lenticule extraction (SMILE).
This article reviews the major SMILE studies on clinical outcomes and those comparing it with LASIK and discusses peri- and postoperative complications.
The Procedure in a Nutshell
Immediately before surgery, the patient fixates on a green blinking light to ensure centration on the optical axis. The eye is docked into a curved contact glass and a low-pressure suction is engaged at the limbus to keep the eye steady.
During the procedure, a femtosecond laser prepares a refractive lenticule within the cornea. The 500KHz laser produces ultrafast laser pulses (10-15 sec.) of near infrared light (1053nm) that conveys approximately 100nJ to 150nJ. Individual laser pulses are focused in the corneal stroma, where plasma expansion leads to localized photodisruption of the tissue. As cavitation bubbles from neighboring laser spots fuse, a well-defined cleavage plane is created within the tissue.
The surgeon places laser pulses in a spiral pattern at a distance of 2µm to 5µm. Initially, the posterior refractive surface of the lenticule is cut (Figure 1a), followed by the anterior surface, which is slightly enlarged to facilitate surgical manipulation. Finally, the surgeon creates a small peripheral incision (2mm to 4mm) from which to extract the refractive lenticule (Figure 1b). The surgeon breaks any remaining tissue bridges with a blunt spatula and uses forceps to grasp and remove the lenticule (Figures 1a and 1d).1-3
SMILE is a one-step laser procedure, where the critical refractive laser treatment is performed on the intact cornea, rather than on the exposed stroma, as in excimer-based procedures, avoiding the potential variability associated with excimer laser photoablation. Furthermore, the minimally invasive SMILE treatment causes very little trauma to the corneal surface and leaves the anterior stroma almost untouched, resulting in less corneal denervation than after LASIK, in theory reducing the negative biomechanical impact.
Internationally, the currently available SMILE procedure allows myopic corrections of up to -10D spherical equivalent refraction, including correction of up to 5D of astigmatism. Hyperopic treatments are not yet available, but studies are ongoing.4,5 In September 2016, the laser was FDA-approved for myopic corrections between -1D and -8D in individuals 22 years or older.
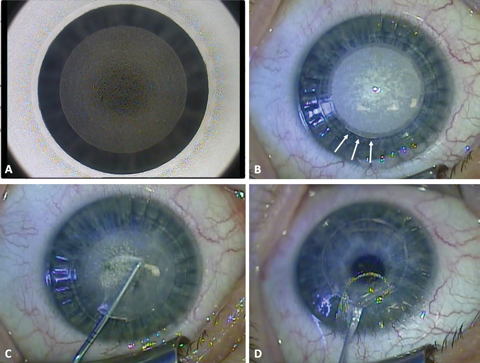 |
| Fig. 1. These images depict the SMILE surgical procedure from start to finish. A) During the laser procedure, the posterior lenticule surface has been cut. B) After the anterior lenticule surface has been cut, a 40-degree incision is created (arrows). C) Next is careful dissection of the lenticule with a blunt Chansue dissector. The superior surface of the lenticule is dissected followed by the posterior surface. D) Finally, the lenticule is extracted through the small periphal incision. Click image to enlarge. |
Choosing the Right Patients
Patient selection is no different for SMILE than for LASIK, although the FDA has placed specific restrictions for patient age and refraction in the United States. Most surgeons use the same precautions for residual stromal thickness in both procedures and, as with LASIK, keratoconus suspects should not be treated with SMILE. Also similar to LASIK, the approximate thickness of the tissue removal is dependent on the diameter of the lenticule and may be approximated using the Munnerlyn formula.6 During pre-examination, clinicians should be aware of stromal scars, as they increase the risk of inadvertent perforation of the anterior stromal cap during surgery. However, with careful dissection of the refractive lenticule, most patients with anterior stromal scars may still be treated with SMILE.
Table 1. Pre- and Postoperative Data | ||||||||||||
| Patient Data | Predictability | Safety | Efficacy | |||||||||
| Patient | Eyes | Follow up | Pre-op SEQ (D) | Post-op error in SEQ (D) | SEQ ±0.5D | SEQ ±1.0D | Regress. (D) | CDVA loss ≥2 lines | Safety Index | UDVA ≥20/20 | Efficacy index | |
| Hansen et al.16* | 411 | 722 | Three months | -6.8 ± 1.7 | -0.4 ± 0.5 | 88% | 98% | - | 2.0% | - | 58% | - |
| Hjortdal et al.7* | 335 | 670 | Three months | -7.2 ± 1.3 | -0.3 ± 0.4 | 80% | 92% | - | 2.4% | 1.07 | 60% | 0.9 |
| Ivarsen et al.17* | 808 | 1,574 | Three months | -7.3 ± 1.8 | -0.2 ± 0.5 | 78% | 95% | - | 1.5% | 1.05 | - | - |
| Liu et al.25 | 57 | 113 | Six months | -5.2 ± 1.7 | 0.0 ± 0.2 | 97% | 100% | n/a | 2.0% | - | 58% | - |
| Reinstein et al.12** | 69 | 110 | One year | -2.6 ± 0.5 | -0.1 ± 0.4 | 84% | 99% | n/a | 0.0% | - | 96% | - |
| Sekundo et al.15 | 27 | 53 | One year | -4.7 ± 1.3 | -0.2 ± 0.2 | 92% | 100% | 0.1 | 0.0% | 1.08 | 88% | 0.99 |
| Pedersen et al.13 | 87 | 87 | Three years | -7.3 ± 1.4 | -0.3 ± 0.6 | 78% | 90% | n/a | 0.0% | 1.13 | 71% | 0.91 |
| Han et al.14 | 26 | 47 | Four years | -6.3 ± 1.5 | 0.0 ± 0.1 | 89% | 100% | n/a | 0.0% | 1.16 | 92% | 1.07 |
| SEQ: spherical equivalent refraction. *Includes learning curve. **Intended slight over-correction. | ||||||||||||
The Results are In
The first SMILE reports were published in 2011, yet the number of clinical studies is still relatively few. Here, we primarily consider studies using the current 500kHz laser with a minimum of 100 eyes or at least a one-year follow up (Table 1).
Refractive outcome. Most studies have examined patients with a preoperative refraction of approximately -6D with varying degrees of astigmatism and follow up. On the whole, about 80% of patients obtain a postoperative refraction within ± 0.5D of the target refraction and roughly 95% of patients obtain a refraction within ± 1.0D.
According to one study, the refractive predictability after SMILE is unrelated to the attempted myopic correction—unlike excimer-based treatments, for which the refractive predictability typically decreases with increasing myopic correction.7,8 Moreover, studies show other parameters, including patient age, gender and preoperative corneal power, have little impact on the refractive outcome after SMILE.7
Only three larger studies evaluate correction of myopic astigmatism in detail. In one study of 775 eyes three months after surgery, 95% of patients had a postoperative spherical equivalent refraction within ± 1.0D of the intended correction.9 However, an astigmatic under-correction of 13% was reported for small cylinders and an under-correction of 16% for large cylinders greater than or equal to 2.5D. A similar astigmatic under-correction of approximately 10% to 15% per diopter was reported in two smaller studies one year after surgery.10,11
Refractive stability. In three studies with one, three and four years of follow up, researchers observed no significant regression.12-14 A fourth study with a one-year follow up found a small regression of 0.08D.15
Following myopic astigmatism correction, investigators note the spherical equivalent refraction, as well as the cylinder, is stable from one week to 12 months post-op.10
Visual outcome. The postoperative uncorrected distance visual acuity (UDVA) is a common measure of the efficacy of a refractive procedure. With SMILE, researchers found an overall UDVA of 20/20 or better in 58% to 96% of individuals from three months to four years post-procedure.12,16 The relatively large variation may be related to differences in the intended target refraction. Thus, an intentional over-correction in some studies will tend to improve the reported efficacy.
Most studies report an efficacy index between 0.9 and 1.0, indicating that patients can expect, on average, an UDVA of 90% to 100% of their preoperative corrected distance visual acuity (CDVA).7,14
After myopic astigmatism correction, one study reports an UDVA ≥20/20 in 55% of patients with small cylinders and 40% of patients with cylinders ≥2.5D.9 Another investigation found an UDVA ≥20/20 in 57% after correction of cylinders from 0.75D to 4.0D, whereas other researchers found 79% to have an UDVA of at least 20/20 after correction of small cylinders.10,11 In general, the observed UDVA after astigmatic corrections mirrored the refractive outcome with poorer outcome in larger cylinders.
Safety. The overall safety of refractive surgical procedures is usually assessed by the induced change in CDVA, where a loss of two or more lines on the Snellen acuity chart is considered significant. Unfortunately, most of the existing studies are too small to properly evaluate SMILE safety. The largest studies all report a two-line loss for between 1.5% and 2.4% of patients after the procedure.7,17 However, these studies all include the initial learning curve of the surgeons, which may have negatively influenced the outcome. Moreover, these studies found a safety index of more than 1.0, indicating that the patients on average had an increase in CDVA—most presumably due to the induced increase in magnification after surgery.7,17
In a study of 1,574 eyes three months after SMILE, 1.5% of patients experienced a two-line loss in CDVA.17 However, when re-examining these patients one to two years later, the researchers noted preoperative CDVA was restored in all eyes, suggesting late recovery of visual acuity can occur in a small subgroup of patients.17
Complications. A number of studies report a variety of perioperative issues with SMILE, although most studies are too small to adequately assess their prevalence (Table 2). In addition, another recent study found the incidence of perioperative complications drops with increasing surgeon experience.18
The most frequently reported complications—such as small epithelial defects, minor tears or bleeding at the incision—have little clinical implication. Occasionally, lenticule extraction may be difficult due to suboptimal cutting of the lenticule caused by either development of an opaque bubble layer or the appearance of black spots. Other rare complications that may affect the postoperative outcome include cap perforation and large tears.
The combination of low suction and a long laser treatment time may cause involuntary eye movements and a loss of suction during the surgery—a complication in 0.8% to 4.4% of surgical cases.15,17,19-22 Excess fluid at the coupling interface and surgeon inexperience are also risk factors for suction loss, as is patient anxiety, highlighting the importance of mental preparation and perioperative reassurance.21
If suction loss occurs after completion of the posterior surface of the lenticule, the treatment usually may be continued immediately. However, if the posterior cut is incomplete, immediate continuation may cause an anterior-posterior shift that negatively affects the refractive outcome. In these cases, the surgeon may postpone surgery, typically for two to three months, and consider an alternative keratorefractive approach such as LASIK or surface ablation.
Most post-op complications have little clinical implication and include dry eye during the first postoperative day, microstriae and increased interface scatter (Table 3). Rare complications include keratitis, severe interface inflammation, epithelial ingrowth and irregular topography. In one study of 1,574 eyes three months after SMILE, researchers found irregular topography in 18 eyes, causing monocular ghost images in six eyes.17
Table 2. Perioperative Complications | |
| Incidence | |
| Epithelial defect at the incision | 0.2% to 11%3,15,17,19,20,37 |
| Minor tear at the incision edge | 2.1% to 6.1%17,19 |
| Bleeding at the incision | 0.9%37 |
| Suction loss | 0.8% to 4.4%15,17,19-21 |
| Opaque bubble layer | 0.7% to 4.4%20,37 |
| Black spots | 0.3% to 3.8%20,37 |
| Lenticule extraction difficulties | 0.9% to 3.8%15,17,37 |
| Central epithelial defect | 0.3%17 |
| Cap perforation | 0.3%17 |
| Large tear | 0.1%17 |
Retreatment
Although SMILE has a high refractive predictability, some patients will experience a clinically significant residual refractive error. While the flap may be lifted to perform an enhancement procedure in LASIK, retreatment after SMILE is more complicated. Possible approaches include re-SMILE at another corneal plane, surface ablation with application of mitomycin C or conversion of the SMILE cap to a LASIK flap with the circle procedure.22-24
Table 3. Postoperative Complications | |
| Incidence | |
| Microdistortions at Bowman’s membrane | 4% to 60%19,38,39 |
| Trace haze | 4.0% to 19%15,17,38 |
| Transient surface dryness | 4.8%17 |
| Late recovery of visual acuity | 1.5%17 |
| Epithelial islands at the interface | 0.6% to 2.0%15,17,19 |
| Fiber or debris at the interface | 0.4%17 |
| Monocular ghost images | 0.4%17 |
| Interface inflammation | 0.3% to 1.6%17,40 |
| Keratitis | 0.3%17 |
SMILE vs. LASIK
At present, only three small, randomized studies and a few meta-analyses compare SMILE with LASIK. In two of the randomized studies, the researchers observed no significant differences between SMILE and LASIK with respect to refractive predictability or efficacy.25,26 SMILE showed less induction of higher-order aberrations (HOAs) in both studies and, in one of them, better postoperative contrast visual acuity and Schirmer scores.26 The third study, however, found that topography-guided LASIK offered better refractive predictability than SMILE.27 This study also found better UDVA and contrast vision after LASIK—both probably due to an under-correction of -0.23D in SMILE eyes.
Two meta-analyses found similar refractive predictability, efficacy and safety after SMILE and LASIK, but SMILE showed better corneal sensitivity and tear film break-up time compared with LASIK.28,29 Another, more recent meta-analysis of 27 comparative studies also found similar clinical outcomes between the two procedures, but favored SMILE with respect to the induction of corneal HOAs.30 Finally, four meta-analyses focused on sensitivity after SMILE and LASIK and found better outcomes in SMILE treated eyes.31-34
Researchers speculate that the nearly intact anterior stroma after SMILE leaves the cornea biomechanically stronger than after LASIK.35 Several studies have attempted to verify this, but with little success, although one meta-analysis suggests SMILE has less negative biomechanical impact than LASIK.29 Still, investigators recently published one case of iatrogenic keratectasia 18 months after SMILE, in a cornea with inconspicuous preoperative topography.36 Thus, it remains unclear whether SMILE offers any biomechanical advantages over LASIK.
What We Do and Don’t Know
The minimal impact on the anterior stroma is one of the most interesting aspects of the SMILE procedure. It spares the stromal nerves, and several studies demonstrate better corneal sensitivity after SMILE than after LASIK. Still, the exact implication of this observation remains unclear. Myopic astigmatism correction is also promising, but hyperopic treatments need further evaluation. The excimer laser still remains the only option in complicated cases, as compensation for eye rotation and aspheric or custom lenticule profiles are still unavailable with SMILE.
Although only available on one laser system (VisuMax, Carl Zeiss Meditec), SMILE will be on everyone’s radar moving forward, as it may eventually allow alternative new treatments, including re-implantation or transplantation of refractive lenticules for refractive or tectonic purposes. Further research will help clinicians better understand SMILE’s place in the refractive surgery armamentarium and help document its evolution.
Dr. Ivarsen is a consultant and associate professor of ophthalmology at Aarhus University Hospital in Denmark.
Dr. Hjortdal is a consultant and clinical professor of ophthalmology at Aarhus University Hospital in Denmark and medical director of the Danish Cornea Bank.
Aarhus University Hospital has specified research agreements with Carl Zeiss Meditec.
1. Sekundo W, Kunert K, Russmann C, et al. First efficacy and safety study of femtosecond lenticule extraction for the correction of myopia: six-month results. J Cataract Refract Surg. 2008;34(9):1513-20. |
Comanaging Refractive Surgery: An OD’s PerspectiveBy , and Many of our patients have thought about refractive surgery at some point, and some seek information directly from a surgery center without consulting their OD. To combat this, we must be proactive and initiate this discussion first to clarify our integral role in the pre- and postoperative care. Patients need to know the refractive surgery process begins with a refractive screening (vision, pachymetry, topography, cycloplegia, etc.) right here in our office. FAQs What is SMILE? It is an alternative to LASIK that some providers view as potentially safer. Essentially, it is a different road to get to the same destination of freedom from glasses. What does the procedure entail? The SMILE procedure uses a flapless laser procedure to address your nearsightedness. Am I a candidate for SMILE? As in any refractive procedure, this will depend on a number of factors such as your current glasses prescription, corneal shape, corneal thickness and ocular health. If you are not an ideal candidate for SMILE, our refractive surgeons can perform several other refractive surgeries such as LASIK, PRK, implantable collamer lens, extended depth of focus intraocular lens and corneal inlays. I’m happy to schedule you for a full refractive consultation to determine which procedure is best. What are the risks? Every surgery involves risk; however, we will work closely with your surgeon to identify which procedure and medications are best for you. How are the outcomes? SMILE has been a very successful procedure provided internationally for many years. According to the FDA clinical study, 88% of patients achieve 20/20 better.1 What is the next step? Let’s schedule a refractive consultation to see if you are a candidate. Partner and Grow Refractive surgery is another opportunity to expand your practice. As you know, happy patients tell everyone. Patients remember who provided their procedure and who was with them from pre-op to post-op success. Make sure you are the doctor everyone is talking about. Recchioni A, Hartwig A, Dermott J, et al. Early clinical outcomes after small incision lenticule extraction surgery (SMILE). Cont Lens Anterior Eye. 2017 Oct 25. pii: S1367-0484(17)30257-6. [Epub ahead of print]. |

