| |
Volume 12, Number 2 |
June 2016 |
|
|
Inside
This Issue |
|
|
|
|
|
This e-newsletter is provided free to doctors through industry support from |
 |
|
FROM
THE DESK OF THE EDITOR
Optometry and the ORS lost a true legend last month, Dr Larry Alexander. Larry was a true pioneer in Optometry, a true leader in the field of posterior segment and retina. He began lecturing and writing about the retina at a time when many ODs were doing little more than refractions, and served as inspiration and a mentor to many who came after him. His pivotal work, Primary Care of the Posterior Segment , remains a fixture in the optometric literature, and I often consult it when preparing a lecture or learning about a specific disease. Larry wore many hats in optometry: professor at UAB for 20 years , educator, author, editor, and industry consultant, most recently with Optovue. But what really set Larry apart was his genuineness and his friendship. Larry truly loved life, and was very devoted to his family, particularly his lovely wife Lynn to whom he was married for over 40 years, and his kids and grandkids. He served as a friend, role model, and mentor to myself and many younger colleagues who were starting to lecture. He was always ready to lend a hand or sage advice to anyone, never wanting or expecting anything in return.
 |
Larry you will be missed. But I for one, as well as many of my colleagues especially here at the ORS, will be thinking of you every time we lecture on the retina. You were truly one of a kind!
Steven Ferrucci, O.D., F.A.A.O.
Editor in Chief
Save the Date
Mark your calendar for December 3-4, 2016. The ORS and Review of optometry are excited about bringing our Annual Retina Update to the Phoenix/Scottsdale, AZ area this year! A distinguished slate of speakers from both optometry and ophthalmology will present clinically relevant information on vitreoretinal disease prevention, diagnosis, technology, and treatment/management. Don't miss optometry's premier posterior segment educational event as we focus on providing education and insight into best retina practices in 2016.
More info to come….. |
PRESIDENT'S MESSAGE
There are simply some people in this world who stand out. They set themselves apart through the impact that they have on the lives of others. By all accounts, our colleague and friend Larry Alexander was one of those people. I am certain that almost everyone would agree that there are not many individuals out there like Larry. His wit, his candor, his smile and his dedication to our profession were unparalleled. Larry was a valued confidant and mentor to me, as he was to many of you. His contributions to our profession are too voluminous to
LIVE
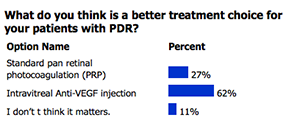
POLL |
Do you perform scleral depression on patients that present with symptomatic PVD?
|
name. Highlights include publication of several editions of Primary Care of the Posterior Segment, a prolonged time spent as an educator of optometry students, Presidency of the ORS, and serving as a section editor for Optometry and Vision Science. In addition, Larry was also heavily involved with industry, helping to promote both education and technological advancements. It is not a stretch to say that if you are an optometrist, or even if you are associated with our profession in some way, then you have been impacted or influenced by Larry. With everything that he did for both his patients and our profession, it is difficult to find a single word that encompasses his impact. I think, however, that in Larry’s case that word would have to be passion. Larry was, if nothing else, unfailingly passionate. Everyone lives,
but Larry lived. And we are all better off because of that. We will miss you my friend.
Brad Sutton, O.D., F.A.A.O.
ORS President

YOU
MAKE THE DIAGNOSIS
Answer appears later in newsletter.

MARCH 2016
POLL RESULTS
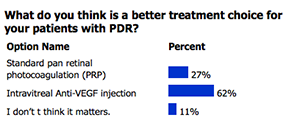
|
CLINICAL
PEARLS
Dilating agents
Joseph Pizzimenti, OD, FAAO
ORS Fellow
1. Hydroxyamphetamine Hydrobromide1.0%/Tropicamide 0.25%
Paremyd (Akorn) is an effective dilating agent for most patients. It combines the effects of the adrenergic agent, hydroxyamphetamine hydrobromide, and the anticholinergic agent, tropicamide. Paremyd provides clinically significant mydriasis with partial cycloplegia. It is excellent for mydriasis in routine diagnostic procedures and in conditions where short term pupil dilation is desired. It works quickly, with onset of action within 15 minutes, reaching maximum effect within 60 minutes. Recovery begins at 90 minutes and complete in 6 to 8 hours for most patients.
2. 1% tropicamide and 2.5% phenylephrine
Phenylepherine is a sympathomimetic drug related to epinephrine, but is much more stable and produces a more lasting response. Used in tandem, this two-drug method
may be reserved for difficult-to-dilate patients and those who present with symptoms consistent with posterior vitreous detachment and retinal breaks/detachments, where maximum mydriasis is necessary.
3. 0.2% cyclopentolate/ 0.1% phenylephrine HCl
Cyclomydril (Alcon) is ideal for dilating young children. It can usually be used on infants
as well. As with all of these dilating agents, be sure to read the precautions and contraindications. Cyclopentolate blocks the action of acetylcholine resulting in relaxation of the iris sphincter muscle. Anticholinergic effects of cyclopentolate produce both mydriasis and cycloplegia, which aids in objective refraction.
4. 10% Phenylephrine
This agent may be used for difficult-to-dilate pupils, breaking posterior synechiae and before cataract surgery. It has no effect on the ciliary muscle, so that mydriasis is achieved without any cycloplegia. When instilled into the conjunctival sac, it causes
powerful mydriasis, in addition to vasoconstriction. Phenylephrine 10% eye drops lead to a faster and more pronounced mydriasis but cardiovascular effects such as hypertension and arrhythmias have been reported.
|

JOURNAL
ABSTRACTS
Analysis of Inner and Outer Retinal Thickness in Patients Using Hydroxychloroquine Prior to Development of Retinopathy
The purpose of this study was to determine whether or not there are signs of early damage in the inner and/or outer retina that precede retinopathy in patients who are taking Hydroxychloroquine.
32 patients, 27 women and 5 men, taking Hydroxychloroquine without evidence of retinopathy were retrospectively reviewed from 2010 to 2015 by studying the patients’ SD-OCT studies. These patients were deemed to be free of retinopathy based on previous normal studies including 10-2 HVF, SD-OCT, FAF, and mfERG during their last two screenings. 27 of the 32 patients were age matched in order to accurately compare retinal layer integrity based on the fact that retinal thickness naturally changes with age. 12 of the 27 age matched patients (mean age of 55.5 years, mean dosage of 359.5 mg) were taking Hydroxychloroquine for less than 5 years (short-term usage) while the remaining 15 patients (mean age of 56.9 years, mean dosage of 330.2 mg) were taking the drug for greater than 15 years (long-term usage). Retinal layer thicknesses were measured by commercial and Stanford pixel-by-pixel segmentation software.
Comparing follow up times of 25 and 52 months (39 month median), there was no statistically significant change in inner retinal thicknesses at different retinal regions between short-term and long-term Hydroxychloroquine users. This finding also held true for outer retinal thickness.
This retrospective review, despite its small sample size, concluded that there is no clinically relevant inner retinal involvement. Additionally, there were no early warning signs of impending retinopathy when studying the outer retinal layers in long-term drug users until actual focal retinal damage ensued. Given these findings, and the known fact that early detection of Hydroxychloroquine retinopathy can limit visual loss by stopping therapy which subsequently prevents significant progression, it is recommended to investigate other manifestations of early retinopathy rather than focusing on progressive retinal thinning. Such screening tools may include the use of topographic SD-OCT thickness maps, which show the location and extent of retinal damage, given that some cross-sectional scans may miss focal damage.
Sisternes, L., Hu, J., Marmor, MF. JAMA Ophthalmol. 2016; 134(5): 511-519
Association Between Oral Fluoroquinolone Use and Retinal Detachment
The aim of this study was to assess the association between oral fluoroquinolone use and the risk for RD, including the rhegmatogenous and exudative types.
Exposure to fluoroquinolones during the risk period (1-10 days before RD surgery) was compared with the control period (61-180 days before RD surgery). The association was also assessed regarding use in the recent (11-30 days) and past (31-60 days) intermediate risk period, type of fluoroquinolone, and type of RD.
Of the 27 540 patients that underwent RD surgery and met the study eligibility requirements, 663 patients with RD were exposed to fluoroquinolones, corresponding to 80 cases exposed during the 10-day risk period (≤10 days before RD) and 583 cases exposed during the control period (61-180 days). The investigators found a significant increased risk for RD during the 10-day period after the dispensing of oral fluoroquinolones, with an adjusted odds ratio of 1.46 (95% CI, 1.15-1.87). Recent use and past use of fluoroquinolones were not associated with a higher risk for RD.
Current oral fluoroquinolone use was associated with an increased risk for RD, including the rhegmatogenous and exudative types. These findings, along with the available literature, suggest an association between oral fluoroquinolone use and the risk for RD. The nature of this association should be further investigated in future studies.
Raguideau F, Lemaitre M, Dray-Spira R, et al. JAMA Ophthalmol. April 2016;134(4):415-421.
Lamellar Macular Hole: Two Distinct Clinical Entities?
The purpose of this retrospective observational case series was to investigate whether macular holes can be divided into different subgroups.
In this institutional study, clinical charts and spectral-domain optical coherence tomography (OCT) images of 102 eyes of 90 consecutive patients diagnosed with lamellar macular hole were reviewed. In OCT imaging, the presence of lamellar macular hole was defined according to the following findings: presence of irregular foveal contour, separation of the layers of the neurosensory retina, and the absence of full-thickness macular defect. Mean outcome was the morphologic and functional characterization of different subtypes of macular hole.
Two different subtypes of lamellar macular hole were identified: tractional and degenerative. The first type, tractional, was diagnosed in 43 eyes, and was characterized by the schitic separation of neurosensory retina between outer plexiform and outer nuclear layers. It often presented with an intact ellipsoid layer and was associated with tractional epiretinal membranes and/or vitreomacular traction. The second type, degenerative, was diagnosed in 48 eyes, and its distinctive traits included the presence of intraretinal cavitation that could affect all retinal layers. It was often associated with nontractional epiretinal proliferation and a retinal “bump.” Moreover, it often presented with early ellipsoidal zone defect and its pathogenesis, although chronic and progressive, remains poorly understood. Eleven eyes shared common features with both tractional and degenerative lamellar macular holes and were classified as mixed lesions.
The study’s conclusion was that degenerative and tractional lamellar macular holes may be 2 distinct clinical entities. The study recommends a revision of the current concept of lamellar macular holes.
Govetto A, Dacquay Y, Farajzadeh M, et al. Am J Ophthalmol. 2016 Apr;164:99-109.
Distinguishing Polypoidal Choroidal Vasculopathy from Typical Neovascular Age-Related Macular Degeneration based on Spectral Domain Optical Coherence Tomography
The purpose of this study was to investigate the sensitivity and specificity of SDOCT in distinguishing polypoidal choroidal vasculopathy (PCV) from typical neovascular age-related macular degeneration (nAMD)
188 eyes in 156 patients with active PCV or typical nAMD were enrolled prospectively. Three SDOCT characteristics were estimated in all the eyes: pigment epithelium detachment, double-layer sign, and thumb-like polyps. A diagnostic test to differentiate PCV from nAMD based on SDOCT was performed. Furthermore, the sensitivity and specificity was validated in a retrospective series of patients. Pigmented epithelium detachment, double-layer sign, and thumb-like polyps were more common in PCV eyes than in nAMD eyes. When the cutoff point was set as at least 2 positive signs out of 3 in the diagnostic test, the sensitivity was 89.4% and specificity was 85.3%. The results of the validation test further confirmed the strategy, with satisfying sensitivity (87.5%) and specificity (86.2%)
In conclusion, spectral domain optical coherence tomography is sensitive and specific in distinguishing PCV from nAMD. From these results, the presence of at least two out of three signs (pigment epithelium detachment, double-layer sign, and thumb-like polyps) indicates a positive test and is therefore suggested to be the screening strategy for PCV
Liu, R, Li, J, Li, Z et al. Retina. April 2016. 36(4): 778-786
Optical Coherence Tomography Features of Active and Inactive Retinal Neovascularization in Proliferative Diabetic Retinopathy
The objective of this study was to describe SDOCT features of retinal neovascularization in proliferative diabetic retinopathy and thus to identify novel signs of new vessel activity.
This retrospective, cross-sectional study collected data over a 9-month period. SDOCT scans were performed over areas of new vessel complexes (NVC) in both the disk and elsewhere, and were qualitatively graded by two masked observers. New vessel complexes activity was determined using clinical and angiographic criteria and correlated with spectral domain optical coherence tomography features.
Forty-three eyes of 30 patients with PDR were included. Sixty-one NVC lesions (NVD—37.7%, NVE—62.3%) were captured by SDOCT and analyzed. Among them, 63.9% were classified as active and 36.1% as quiescent. Five distinctive features were identified as significantly different between active and quiescent NVC: the presence of vitreous hyper-reflective dots was the only predictive for active NVC (P = 0.002); whereas the presence of epiretinal membrane (P = 0.04), inner retinal tissue contracture (P = 0.03), vitreous invasion (P = 0.02), and protrusion towards vitreous (P = 0.002) indicated quiescent NVC.
In this exploratory study, the presence of vitreous hyperreflective dots, epiretinal membrane, inner retinal tissue contracture, vitreous invasion, and vitreous protrusion were identified as distinct OCT features that may be used to differentiate active from quiescent NVC. Such parameters may be useful as a noninvasive imaging modality in eyes undergoing treatment for PDR.
Vaz-Pereira S, Zarranz-Ventura J, Sim DA, et al Retina. 36(6):1132-1142, June 2016.
Detection of Myopic Choroidal Neovascularization Using Optical Coherence Tomography Angiography
The purpose of this study was to assess whether OCT angiography (OCTA) can be used as an alternative to conventional fundus angiography (FFA) for the detection of myopic choroidal neovascularization.
Twenty-eight eyes of 26 consecutive Japanese patients with exudative lesions associated with pathologic myopia were included in this institutional study. Myopic CNV was detected in 23 eyes of 22 patients; 5 eyes exhibited simple hemorrhage. The main outcome measure was CNV detection by OCTA and FFA. The CNV area was individually measured by FFA and OCTA. Intraclass correlation coefficients (ICCs) for the CNV area, independently measured by 2 investigators using OCTA and FFA, were also determined.
OCTA images with sufficient quality for CNV assessment were obtained for 17 eyes with CNV and 4 without. FFA alone detected CNV in all 17 eyes, while OCTA alone detected CNV in 16 (94.1%). The 1 eye for which CNV was not detected by OCTA exhibited a 0.01 mm2 area on FFA. Both FFA and OCTA did not detect CNV in eyes with simple hemorrhage. The mean CNV areas on FFA and OCTA were 0.59 ± 0.56 mm2 and 0.51 ± 0.55 mm2, respectively; the 2 values were significantly correlated (P < .001, r = .86). The ICC (2, 1) values for FFA and OCTA were 0.944 and 0.997, respectively.
The results indicate that OCTA can detect most myopic CNVs if high-quality images are acquired and can preclude the requirement for FFA in these settings.
Miyata M, Ooto S, Hata M, et al. Am J Ophthalmol. 2016 May;165:108-14.
Early Disease Manifestations of Macular Telangiectasia Type 2
To purpose of this study was to report very early morphologic and functional changes in patients with macular telangiectasia type 2.
Patients with asymmetric disease manifestations, in whom retinal alteration characteristic for macular telangiectasia type 2 were present in one but not in the apparently unaffected fellow eye, underwent multimodal imaging and functional testing (microperimetry, visual acuity, reading ability, Amsler test)
Fellow eyes not allowing the diagnosis of macular telangiectasia type 2 based on hitherto diagnostic standards consistently showed a severely reduced directional cone reflectance (Stiles–Crawford effect).
Optical coherence tomography revealed an asymmetric configuration of the fovea pit with focal temporal thinning most pronounced at 1 degree eccentricity.Topographically related, macular pigment optical density was reduced in a small wedge-shaped temporal paracentral sector, resulting in an increased signal on fundus autofluorescence and fluorescein angiography imaging. No functional deficits were detectable in fellow eyes. Haidinger brushes were perceived in the fellow eye but not in the affected index eye with pronounced loss of macular pigment.
In conclusion, specific morphologic alterations precede vascular alterations and functional deficits in macular telangiectasia type 2. The described changes indicate a primarily degenerative process with a secondary retinal vascular phenotype, and may be helpful for early identification of patients and affected family members
Charbel PI, Heeren P, Tjebo FC et al. Retina. March 2016. 36(3): 524-534
Laser Prophylactic Treatment of the Fellow Eye in Giant Retinal Tears: Long-term Follow-up
The purpose of this study was to observe the outcomes of patients who had giant retinal tears (GRT) and subsequently had prophylactic laser treatment in the fellow eye versus those who were solely observed. GRTs are full-thickness retinal breaks extending for at least 90 degrees of the retinal circumference, and often have devastating visual consequences.
160 patients who had previous surgical treatment for GRTs in one eye were retrospectively reviewed between January 1989 to December 2005. 62 patients’ fellow eyes were observed while the other 98 patients’ fellow eyes were treated with 360 degrees of prophylactic laser. 72 of the 98 treated patients received Argon laser while the other 26 received green diode laser. The mean follow-up for the observation group was 43.5 +/- 19.8 months and 37.2 +/- 16.3 months for the treatment group.
In the observation group, the incidence of smaller retinal tears with localized pre-equatorial retinal detachments was 3.2%, while it was 11.2% in the treatment group. The incidence of GRTs with macula-on RDs was 0% and 2% in the observation and treatment groups, respectively. Incidence of GRTs with macula-off RDs was 14.5% in the observation group and 0% in the treatment group.
Interestingly, the incidence of new retinal tears between the two groups was similar, however, patients in the treatment group developed less GRTs and did a better job in confining the retinal detachment and avoiding macula-off RDs altogether. Prophylactic laser eyes ultimately just needed adjuvant laser treatment and rarely pars plana vitrectomy, while patients who were observed were more likely to progress to macula-off RDs and needed subsequent PPV. As a result, prophylactically treated eyes showed a better visual outcome at the final follow up compared with the observation group.
Ripandelli, G., Rossi, T., Cacciamani, A., et al. Retina. May 2016. 36(5): 962-966.
Long-term Evolution of Dome-shaped Macula: Increased Macular Bulge is Associated with Extended Macular Atrophy
The purpose of this article was to analyze the course of dome-shaped macula (DSM), including the development of serous retinal detachments, RPE atrophy, and DSM bulge increase. DSM is an anomaly found in myopic eyes that is thought to be due to perimacular extension of the myopic staphyloma.
29 myopic eyes (19 patients: 16 women and 3 men) with DSM were retrospectively studied between 2005 and 2014 by reviewing their clinical data, fundus color photographs, FAs, and OCT studies. The age range was between 26-89 years with an average axial length of 27.00 +/- 2.82 mm and refractive error of -7.80 +/- 4.80 D. The average follow up time was 37.89 +/- 33.04 months, ranging from 6 to 111 months. Upon reviewing the studies, all macular changes were noted, including the height of the macular bulge, the extent of RPE atrophy, progression of serous retinal detachments, macular pucker, CNVM, subretinal pigmentary clumps, and flat irregular PEDs.
The height of the DSMs significantly increased, from an initial mean height of 338.9 um to 364.3 um. Of note, this increase was not correlated with the axial length of the patient. Initially, 15 of the 29 (51%) eyes presented with a serous retinal detachment (SRD). 4 of those 15 patients (27%) showed progression, 7 spontaneously resolved (47%), 3 developed new a SRD (20%), while only 1 remained stable (7%). Various treatments including intravitreal IVA, IVTA, PDT, focal laser, and oral eplerenone were given, with essentially no regression or resolution of SRD during or after the treatment period. The extent of RPE atrophy correlated with the height of the macular bulge. Overall, the mean vision remained stable.
This retrospective review displayed that despite progressive changes in DSM, such as bulge increase with RPE atrophy, visual acuity may remain stable for years. In addition, with the presence of a relatively thickened central choroid and sclera as well as flat, irregular PEDs, it is noted that DSM and CSCR share many clinical characteristics. However, given the unsuccessful treatments of the SRD in this study, the likelihood of the pathophysiology being solely vascular leakage is unlikely.
Soudier, G., Gaudric, A., Gualino, V. et al. Retina. May 2016; 36(5): 944-952.
Fellow Eye Comparisons for 7-Year Outcomes in Ranibizumab-Treated AMD Subjects from ANCHOR, MARINA, and HORIZON (SEVEN-UP Study)
A multicenter cohort study, predetermined secondary analysis of the ANCHOR, MARINA, and HORIZON (SEVEN-UP Study). The purpose of the study was to compare the fellow eyes in subjects with age-related macular degeneration (AMD) for 7-year outcomes arising from contrasting treatment histories and disease statuses.
Exudative fellow eyes remained at risk for further vision decline in later years under management with low-frequency anti-VEGF therapy. In patients with bilateral exudative AMD at baseline, final vision at year 7 was significantly better in study eyes than in fellow eyes, and MA was less severe. Macular atrophy area correlated with final visual outcomes, determined inter-eye vision differences, and was not attributable to high-frequency ranibizumab therapy.
For this cohort of patients with AMD receiving ranibizumab as participants in the original phase 3 clinical trials, study eyes and fellow eyes were compared over the 7-year study period to evaluate rates of exudative disease onset, long-term visual outcomes resulting from contrasting treatment histories, and progression of MA.
In summary, study eyes with a treatment history of 2 years of intensive intravitreal ranibizumab had better long-term vision outcomes than exudative fellow eyes, for which anti-VEGF therapy was initially prohibited. Exudative fellow eyes did not reach a “burnt-out” stage, but instead showed continued vision decline in the later years of the study period under low-frequency anti-VEGF treatment, suggesting that persistent anti-VEGF treatment for advanced-stage exudative AMD may be ameliorative. In addition, MA was less severe in the study eyes than in the exudative fellow eyes, indicating that high-frequency ranibizumab did not lead to unfavorable MA progression over time.
Bhisitkul RB, Desai SJ, Boyer DS, et al.Ophthalmology 2016;123:1269-77.

Ranibizumab 0.5 mg treat-and-extend regimen for diabetic macular oedema: the RETAIN study
The purpose of this study was to demonstrate non-inferiority of intravitreal ranibizumab injections (Lucentis ®; Genentech, Novartis Pharma AG) with or without laser treatment on a treat-and-extend (T&E) protocol vs a pro-re-nata (PRN) protocol in a population of individuals with diabetic macular oedema (DMO). The primary outcome was best-corrected visual acuity (BCVA).
A total of 372 individuals were enrolled in the study and randomized to the following three treatment strategies: 1) T&E + laser (n=121), 2) T&E (n=128), or 3) PRN (control; n=123). The PRN injections were completed on a basis of DMO affecting BCVA and was left to the discrimination of the treating physician.
Both treatment strategies including the T&E practice were shown to be non-inferior to PRN group of ranibizumab intravitreal injections in terms of BCVA from baseline to follow-up. The T&E protocols resulted in an average of 46% fewer clinic visits, but did have a slightly higher average number of injections than the PRN group.
In conclusion, intravitreal ranibizumab injections on a T&E basis are non-inferior as a treatment strategy for managing DMO when compared to being done PRN. In addition, the T&E strategy reduced the number of clinic visits though it did require more frequent injections.
Prünte C, Fajnkuchen F, Mahmood S, et al. Br J Ophthalmol. 2016; 100:787-795.

|
ANSWER
TO "YOU MAKE THE DIAGNOSIS"
Paracentral Acute Middle Maculopathy
This patient, a 78 year old Caucasian female with longstanding dry macular degeneration, presented with an acute onset paracentral scotoma in the right eye. Her visual acuity remained unaffected at 20/20. Her medical history was significant for hypertension, which was well controlled on losartan and metoprolol. The images shown are consistent with a diagnosis of paracentral acute middle maculopathy (PAMM), unrelated to the AMD.
The proposed cause of PAMM is ischemia of the retinal deep capillary plexis. Patients with PAMM present with sudden onset of a paracentral scotoma that may or may not affect visual acuity. The appearance of these lesions varies but is most often gray or white. In some cases, the lesion cannot be appreciated funduscopically and is noted only on OCT. PAMM can occur isolated or in conjunction with retinal vasculature disease such as diabetic retinopathy, vascular occlusion or sickle cell disease. In isolated PAMM lesions, the reported associations include flu-like illness, migraines, increased caffeine intake, systemic shock, oral contraceptives and vasopressors. PAMM may also develop idiopathically in young, healthy patients.
The advent of multimodal imaging, in particular SD OCT, has allowed for better detection and understanding of PAMM. When it was initially recognized by Sarraf and colleagues in 2013, it was described as a variant of acute macular neuroretinopathy (AMN). Now SD OCT has allowed us to differentiate these as two separate disorders. In the acute stage, PAMM lesions are characterized by a hyper-reflective band located at the junction of the outer plexiform layer (OPL) and inner nuclear layer (INL). The lesion eventually develops atrophy and thinning of the INL. AMN lesions are located slightly deeper at the OPL and outer nuclear layer (ONL) junction and result in atrophy of the ONL and photoreceptor integrity line (PIL).
Near infrared reflectance imaging can also be used to better visual PAMM lesions. With this testing lesions appear dark or gray. Fluorescein angiography is of little use as the angiograms are often normal. OCT angiography offers a more promising tool to study PAMM, as unlike fluorescein angiography, it allows imaging of the retinal microvasculature. On OCT angiography old PAMM lesions correspond with loss of the deep and intermediate capillary plexuses.
There is no treatment for PAMM. Management involves identifying and treating vascular and systemic risk factors, if present. PAMM lesions resolve over the course of several weeks and eventually develop atrophy of the INL that can only be appreciated via OCT. This corresponds with a persistent scotoma that generally does not improve.
Anna Bedwell, OD, FAAO
|

IN THE
NEWS
 |
AngioVue imaging system receives clearance from FDA
The FDA has cleared the AngioVue imaging system, Optovue announced in a press release.
The device is now commercially available in the U.S.
AngioVue provides physicians with a noninvasive method of visualizing abnormal blood cells in the retina to help determine an appropriate course of treatment.
“We are thrilled to announce FDA clearance for our AngioVue system, which will bring significant benefits of our innovative, noninvasive retinal imaging to patients in the U.S. suffering from retinal diseases that lead to progressive blindness,” Jay Wei, founder and CEO of Optovue, said in the release
|
 |
Gene therapy improves VA in eyes treated for choroideremia
An adeno-associated virus vector improved visual function in two of six patients treated for choroideremia, according to a letter published in the New England Journal of Medicine.
The letter summarized results of a study conducted at the University of Oxford, U.K.
“Best corrected visual acuity is a reliable marker of visual function. In contrast to Leber’s congenital amaurosis, in which visual acuity is generally profoundly affected early in life, choroideremia and most types of retinitis pigmentosa are characterized by progressive loss of the visual field, with visual acuity remaining close to normal levels until the very late stages of disease. Therefore, in some patients, the effect of preserving visual acuity with the use of retinal gene therapy may take several years to become apparent,” the authors wrote.
Investigators injected AAV.REP1, a non-mutated form of CHM in an adeno-associated virus (AAV) vector, into the vicinity of the retinal pigment epithelium and photoreceptor cells.
Injected volumes of AAV.REP1 were 0.1 mL and 0.06 mL.
Results showed that early visual improvement in two of the six patients was sustained at 3.5 years after treatment, despite progressive degeneration in non-treated control eyes.
At 3.5 years, ETDRS visual acuity increased by 21 letters, or more than four lines, from baseline in one patient and by 18 letters, more than three lines, in the other patient.
VA in the respective patients’ control eyes decreased by 18 letters and six letters.
The other four patients had good baseline VA and had limited potential improvement.
One patient developed cataract at 2 years; the patient’s VA at 3.5 years was similar to the value reported at 12 months after treatment, before the cataract was visually significant, the authors wrote.
|
 |
Gene therapy may improve visual function in retinal degeneration caused by RPE65 mutations
An adeno-associated virus vector improved one or more measures of visual function in patients with retinal degeneration resulting from RPE65 mutations, according to a study in Ophthalmology
Investigators set out to assess the safety of rAAV2-CB-hRPE65, a recombinant adeno-associated virus vector expressing RPE65, a 65-kDa isomerohydrolase produced by retinal pigment epithelium cells. Mutations of RPE65 are believed to result in a severe deficiency of active chromophore and can cause Leber congenital amaurosis and severe early childhood-onset retinal dystrophy.
The open-label, nonrandomized, multicenter phase 1/2 clinical trial included 12 patients between the ages of 6 years and 39 years with Leber congenital amaurosis or severe early childhood-onset retinal dystrophy resulting from RPE65 mutations.
The poorer-seeing eye of each patient underwent vitrectomy and received a subretinal injection of rAAV2-CB-hRPE65 at one of two doses of vector genomes.
Treatment was well tolerated in all patients, and no treatment-related serious adverse events were reported.
Adverse events related to vitrectomy included subconjunctival hemorrhage in eight patients and ocular hyperemia in five patients. Adverse events possibly related to the vector agent included ocular hyperemia in two patients and photopsia in one patient.
Best corrected visual acuity improved to pretreatment levels or better by day 14 in two patients, by month 1 in three patients and by month 2 in one patient. Improvements persisted for 2 years in five patients. Three patients experienced an improvement in kinetic visual field area.
BCVA decreased in one patient, and kinetic visual field area decreased in two patients.
|
 |
Clearside’s triamcinolone acetonide formulation achieves primary endpoint in phase 2 clinical trial
Clearside Biomedical reported in a press release that its triamcinolone acetonide formulation candidate Zuprata achieved its primary endpoint of reducing the need for Eylea retreatments in patients with macular edema associated with retinal vein occlusion.
In the phase 2 masked, controlled Tanzanite trial, participants were randomized to receive either intravitreal Eylea (aflibercept, Regeneron) alone or both intravitreal Eylea and suprachoroidal triamcinolone acetonide at the same time, according to a press release.
Preliminary results revealed that patients who received both Eylea and Zuprata qualified for 60% fewer intravitreal Eylea retreatments than those in the control group during the 3-month observation period after initial injection (P = .013).
Furthermore, best corrected visual acuity was improved more in the Zuprata group than in the control group: 19 letter improvement vs. 11 letter improvement, according to the release.
“Based on these results, Clearside intends to follow a 505(b)(2) NDA regulatory approval pathway and expedite the preparations for a Zuprata phase 3 registration program for the treatment of macular edema associated with RVO,” Clearside president and CEO Daniel H. White said in the release.
|
 |
Patients with wet AMD would opt for high treatment burden to prevent worse visual acuity
Patients with neovascular age-related macular degeneration were willing to opt for a higher treatment burden, which included regular intravitreal injections at short intervals and long periods of waiting, treatment and traveling, to prevent worsening of visual acuity, according to a study conducted in Germany and published in Ophthalmology.
Two hundred eighty-four patients were included in the discrete choice experiment. All patients had wet AMD, had received at least one intravitreal injection and were at least 50 years old. Researchers conducted telephone interviews with the subjects.
At study inclusion, 22.9% of patients had poor visual acuity, 54.9% of patients had moderate visual acuity, 14.1% of patients had good visual acuity, and visual acuity was not available for 8.1% of patients.
The attribute “change of VA” influenced overall decisions for or against treatment in 73.6% of patients, “waiting, treatment and travel time” influenced decisions in 21% of patients, and “treatment scheme” influenced decisions in 5.4% of patients.
Overall, patients were willing to opt for an additional 12.7 hours of time spent for each physician visit to achieve stable visual acuity rather than worse acuity. Patients were willing to opt for an additional 21.1 hours spent for each physician visit to improve visual acuity. Each physician visit was defined as including longer waiting, treatment and travel times.
|
 |
Single-fragment antibody VEGF inhibitor meets primary endpoint of non-inferiority
The small compound may allow for more targeted and less frequent injections to treat wet AMD.
A humanized single-chain antibody fragment VEGF inhibitor to treat neovascular age-related macular degeneration was found to be non-inferior to ranibizumab intravitreal injections, according to a phase 2 multicenter study published in Ophthalmology.
The manufacturing of the single-fragment antibody RTH258 (formerly ESBA1008) is a collaborative venture between Alcon and Novartis.
The dose-escalation study, which appeared in Ophthalmology, compared a single intravitreal injection of RTH258 in four doses — 0.5 mg (11 patients), 3 mg (31 patients), 4.5 mg (47 patients) and 6 mg (44 patients) — with a single injection of Lucentis (ranibizumab, Genentech) 0.5 mg (61 patients).
The study also found that the 6 mg dose of RTH258 provided the most potent effect.
The two secondary endpoints were vision and duration of RTH258, both of which were encouraging. Specifically, the median time to post-baseline therapy was 60 days for the 4.5 mg group and 75 days for the 6 mg group, compared with 45 days for ranibizumab.
No adverse events of concern were found for any of the four doses of RTH258.
Furthermore, an extension of the same trial concluded that 50% of patients could be given an injection of RTH258 once every 12 weeks.
|
 |
Pseudodrusen associated with development of neovascular AMD in fellow eye
The presence of pseudodrusen correlated with an increased incidence of neovascular age-related macular degeneration and geographic atrophy in fellow eyes of patients with unilateral neovascular AMD, according to a study in Ophthalmology.
The authors assessed the relationship between pseudodrusen and late AMD in the fellow eyes of patients with unilateral neovascular AMD. Data were culled from the Comparison of Age-Related Macular Degeneration Treatments Trials.
The cohort analysis included 620 fellow eyes of CATT participants with unilateral neovascular AMD and no neovascular AMD or geographic atrophy in the fellow eye at baseline.
At baseline, 176 of 620 fellow eyes (28.4%) had pseudodrusen; 96 (54.5%) had dot pseudodrusen, 145 (82.4%) had reticular pseudodrusen, and 61 (34.7%) had confluent pseudodrusen.
Neovascular AMD developed within 2 years in 54 eyes with pseudodrusen (30.7%) and in 72 eyes without pseudodrusen (16.2%). The difference was statistically significant (P < .0001).
Geographic atrophy developed in 27 eyes with pseudodrusen (15.3%) and in 37 eyes without pseudodrusen (8.3%); the difference was statistically significant (P = .01).
There was an independent association between dot pseudodrusen and neovascular AMD and between confluent pseudodrusen and geographic atrophy.
|
 |
Acucela, University of Manchester enter licensing agreement for gene therapy
Acucela has entered into an exclusive licensing agreement with the University of Manchester to develop and commercialize the university’s human rhodopsin-based optogenetic gene therapy to treat retinitis pigmentosa and related conditions, according to a company press release.
“We are extremely excited to enter into this collaboration with the University of Manchester and to begin the important development work needed to unlock the potential of optogenetic gene therapy to improve visual function in patients who have lost much of their vision as well as their hope,” Ryo Kubota, MD, PhD, chairman, president and CEO of Acucela, said in the release.
The gene therapy will be studied across a variety of genetic mutations in retinitis pigmentosa and related conditions. Acucela plans to evaluate the technology to restore some vision in patients who are legally blind.
|
 |
ThromboGenics enters into exclusive licensing agreement with Galapagos
ThromboGenics has signed an exclusive licensing agreement with Galapagos to develop and commercialize integrin antagonists to treat diabetic eye disease, according to a press release.
ThromboGenics will pay a €1 million upfront technology transfer payment to Galapagos, and Galapagos will receive development and commercial milestone payments and royalties based on any future net sales from products that originated from Galapagos’ library of integrin antagonists.
“We are pleased to have signed this in-licensing deal with Galapagos, which will provide us with access to a collection of integrin antagonists, an exciting class of drugs being developed for back of the eye disease,” Patrik De Haes, MD, CEO of ThromboGenics, said in the release. |
 |
Visunex receives FDA clearance for PanoCam Pro wide-field imaging system
The PanoCam Pro wide-field imaging system has received FDA clearance for the imaging of newborn infants, Visunex Medical Systems announced in a press release.
The wireless imaging system has the capability to detect external, anterior and posterior segment vision disorders in newborns.
“Our PanoCam Pro and PanoCam Review software will help clinicians identify vision disorders that may be reversed to preserve healthy vision,” Wei Su, PhD, CEO of Visunex, said in the release.
|
 |
ForeseeHome AMD monitoring program available for Medicare patients in US
The ForeseeHome AMD monitoring program is available by prescription for eligible Medicare patients in the U.S. who have dry age-related macular degeneration and are at risk for developing wet AMD, Notal Vision announced in a press release.
“Notal Vision is extremely pleased to achieve this significant milestone with the ForeseeHome AMD monitoring system. We have worked diligently for almost 2 years with the goal of ensuring this device is available to eligible patients enrolled in Medicare,” Barak Azmon, MD, CEO of Notal Vision, said in the release.
The Home Monitoring of the Eye study, which helped to establish the system’s clinical utility, evaluated whether the ForeseeHome monitoring system was able to detect wet AMD earlier than standard of care. Results showed that 94% of patients who used the system and progressed to wet AMD maintained vision of 20/40 or better.
|

MEET
THE FELLOWS
In each issue, a Fellow of the Optometric Retinal Society is highlighted. In this issue, Dr. Len Koh, a new ORS fellow, will be highlighted
Len Koh is an assistant dean of clinical affairs and associate professor at Arizona College of Optometry at Midwestern University.
Dr. Koh earned his Doctor of Optometry (O.D.) degree at the New England College of Optometry in Boston, Massachusetts, and completed his postdoctoral residency in primary care at the Pennsylvania College of Optometry in Philadelphia. Dr. Koh completed his Master of Business Administration (M.B.A.) degree in Health Care Administration from Western Governors University in Salt Lake City, Utah. He is currently a Fellow of the American Academy of Optometry (FAAO) and has published numerous articles.
Dr. Koh obtained his Ph.D. in Pharmacology at the University of Toronto in Canada and did postdoctoral fellowships at National Institutes of Health.
In his free time, Dr. Koh likes to read and travel with his family.
WHY
BECOME AN ORS FELLOW?
By Bill Denton, O.D., F.A.A.O.
Chair, Membership Committee
At some point in your career, you realize you just may be coasting. Your knowledge has been limited to the journals you receive and attempt to read, and the conferences that may not be as fulfilling as they once were. You simply need a challenge that will add an extra dimension to your professional learning.
Fellowship in the Optometric Retina Society (ORS) can provide several benefits in addition to the initial challenge of qualifying for this honor. Plenty of perks accompany your induction, but the coolest part is being associated with a body of knowledge and resources which can help you in many other ways. It is not uncommon to receive weekly thought-provoking emails about challenging cases and treatment dilemmas. Some fellows like to share their awesome cases they have diagnosed, while others post their cases with hopes that other Fellows will suggest an alternative differential diagnosis. At times it is like a round-table of brainstorming, but through the use of modern technology. Fellowship has little obligation with a huge opportunity for professional growth.
If you are up to the challenge of becoming a Fellow of the ORS, feel free to peruse the details and application at www.optometricretinasociety.org. Advice can be given to assist you in your quest. Feel free to contact us. |

SPONSOR NEWS

Editor
in Chief
Steven Ferrucci, OD, FAAO
Co-Editor
Mark T. Dunbar, OD, FAAO |
Journal
Reviewers
Philip Kim, OD
Alison Bozung, OD
Leslie Small, OD
Paul Hammond, OD
Nabila Gomez, OD
Elliot Brafman, OD
Senior Graphic Designer
Matt Egger
|
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|