| |
Volume 12, Number 3 |
October
2016 |
|
|
Inside
This Issue |
|
|
|
|
|
This e-newsletter is provided free to doctors through industry support from |
 |
| |
FROM
THE DESK OF THE EDITOR
I recently returned from vacationing in Punta Cana , Dominican Republic, with my family and 26 of our closest friends. We had a great time, with lots of beaching , boating, eating, and relaxing. Overall a huge success. One thing we did while there was tour a cigar factory, one of the largest in the Dominican. The place was huge, as they produce 125,000 cigars a day, both hand rolled and by machine for the less expensive cigars, 60% of which are exported to the US. Further, they had a huge humidor which stored over 6,000,000 cigars. Watching them hand roll the cigars, with the painstaking care to detail they displayed , was impressive. What was slightly disappointing however is that while a premier cigar roller can roll 400-450 cigars per day, at an average selling price of $8-$10 apiece, the top rollers only make $600 a month! It really makes you appreciate where most of us live, and the advantages we have from being optometrists that are able to provide for ourselves and our families. Sometimes, it is good to sit back and be happy for what we have.
LIVE
POLL
|
In light of the June 2016 Revised Recommendations s for screening for plaquenil retinopathy by the Academy of Ophthalmology, which do use?
|
|
Also I recently acquired an Eildon True Color Confocal Scanner by Centervue with Fundus Autofluorescent (FAF) capabilities . The base unit has been available for some time, with the FAF capabilities just released this month. I am told I am the first OD in the US to have the unit! For those of you that do not know, FAF uses various filters to highlight lipofuscin, which is a by-product of cell death, and is released when the retina is under stress or dying. I think the FAF will be great for looking at conditions such as CSR and AMD, especially geographic atrophy, as well as other retinal conditions. I also think that if we get additional treatment for dry AMD, as there are a few in the pipeline, FAF will come increasingly important to differentiate those lesions most amenable to treatment. I have only had it for about 2 weeks, and am very impressed with the images, both color and FAF, as well as the montage feature that allows a great overall view of the retina. It is fully automated, as is the base model, and requires little to no training for your staff. I typically dilate my patients, but the unit can be used with an undliated pupil and is still able to get great images. So if you are looking for a new retina camera, check it out (by disclosure, I do some consulting with Centervue).
Please think about joining us in December for our annual ORS meeting. Joe Pizzimenti has put together a great schedule of speakers, and the venue of Scottsdale in December is enticing!
Steven Ferrucci, O.D., F.A.A.O.
Editor in Chief
|
ORS 2016 ANNUAL MEETING
Mark your calendar for our Annual Retina Update, open to all eye care providers! The dates are December 2-4, 2016. ORS and Review of Optometry are excited about bringing this unique and innovative CE program to the world class Westin Kierland Resort & Spa in Scottsdale, Arizona.
A distinguished slate of speakers from both optometry and ophthalmology will present clinically relevant information on vitreoretinal disease prevention, diagnosis, technology, and treatment/management. Register early to sign up for a hands-on workshop using the most cutting edge diagnostic technology. Don't miss optometry's premier posterior segment educational event as we focus on providing education and insight into best retina practices in 2016.
For details including conference agenda, speakers, hotel info, and registration, visit http://jobson.cvent.com/events/retina-update-2016/event-summary-e629bfb8ca6f467292eeb4bb0e83af16.aspx.
|
PRESIDENT'S MESSAGE
Coming up December 2-4 in Scottsdale, Arizona, the ORS will once again be hosting our annual Retina Update meeting in conjunction with our friends and partners at Jobson / Review of Optometry. For those of you who are interested in the posterior segment, I highly encourage you to consider attending this traditionally informative and engaging meeting. As always, several excellent speakers will be featured, presenting on a wide range of clinically relevant topics. Make no mistake, this meeting is for practitioners. Our goal each year is to provide cutting edge vitreoretinal education that enhances optometrists’ ability to take excellent care of their patients. That is, after all, part of the driving mission of the ORS. I am particularly excited that we have added a hands on technology workshop on Friday evening this year. It will allow attendees to gain first-hand experience with cutting edge diagnostic instruments and management tools. Workshops such as this have been very well received at other meetings hosted by Jobson, and I am certain that this one will be as well. So, if you have an interest in the retina and the vitreous, and you need some continuing education, come and join us in Arizona!
JUNE 2016
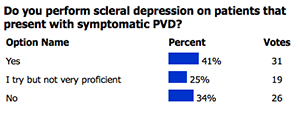
POLL RESULTS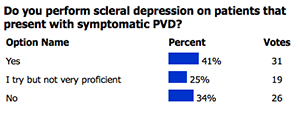
|

YOU
MAKE THE DIAGNOSIS
Answer appears later in newsletter.

CLINICAL
PEARLS
Home Amsler Grid
By: Jeffry Gerson, OD, FAAO
ORS Fellow
Home vision testing is here...but not just what you hear about in the news for an eye exam replacement. We know from various studies in AMD that when CNVM is caught earlier, people have a better outcome with treatment. There are 2 FDA approved home testing regimens. The ForSee Home from Notal Vision, as was tested as part of the AREDSII trial, is one option for patients. This is even covered, in part, by Medicare. It is a desk-top device that is shipped to patients from Notal. The other test is the mVT from Visual Arts and Science is an app for most iPhones or Androids. It is not covered by medicare, so there is a nominal fee to the patient. Both tests use vernier acuity, and may be able to detect very minimal changes in vision long before traditional testing with an Amsler grid would. For more information you can go to:
www.forseehome.com for information on ForSee Home
www.myvisiontrack.com for information on mVT
Which agent is best for DME? A look at DRCR.net Protocol T
Leo Semes, OD, FAAO
ORS Fellow
We may be confronted with the patient who has experienced sudden painless vision loss and be in the position of distinguishing between AION and CRAO. The OCT can provide the information to make the call. In CRAO the thickness of the RNFL will be severely attenuated whereas in the case of a previous AION, RNFL attenuation will be to a lesser extent. Being able to distinguish between these two etiologies may be moot in the eyes of some (no pun, patient or provider) but the systemic management can be guided more specifically.
Reference: Dotan G, Goldenberg G, Kesler A, Naftaliev E, Loewenstein A, Goldstein M. The Use of Spectral-Domain Optical Coherence Tomography for Differentiating Long-standing Central Retinal Artery Occlusion and Nonarteritic Anterior Ischemic Optic Neuropathy. Ophthalmic Surgery, Lasers and Imaging Retina2014; 45 (1) : 38-44. |

JOURNAL
ABSTRACTS
Risk Factors Associated with the Ophthalmoscopic Findings Identified in Infants with Presumed Zika Virus Congenital Infection
Although Zika Virus (ZIKV) was first identified in humans in 1953, the recent epidemic in Brazil led to the discovery of viral-associated central nervous system malformations such as microcephaly after presumed intrauterine infection. Early reports of funduscopic abnormalities have sparked investigation of the potential risk factors that contribute to ocular involvement in patients exposed to ZIKV, which is the subject of this cross-sectional study.
40 Brazilian infants with suspected or confirmed microcephaly were enrolled in the study after serological testing ruled out toxoplasmosis, syphilis, rubella, cytomegalovirus, human immunodeficiency virus, and herpes simplex virus. Using IgM antibody-capture ELISA (MAC-ELISA), 24 infants had cerebrospinal fluid (CSF) tested for ZIKV and dengue fever virus (DFV). The remaining 16 infants did not receive confirmatory MAC-ELISA because of unexpected unavailability of the test in December 2015.
The participants were divided into two groups: infants with ocular involvement and infants without involvement. The main findings were mild pigment mottling with loss of foveal reflex (55%) and optic disc hypoplasia (17.5%). There were only two variables associated with an increased risk of ocular involvement: (1) mothers who experienced flu-like symptoms (i.e. rash, fever, headache, arthralgia) during the first trimester of pregnancy, and (2) smaller cephalic diameter at birth. There was otherwise no significant difference between birth term, gender, delivery type, maternal age, birth weight, or ocular axial length.
As in other congenital infections, such as toxoplasmosis, infants are most susceptible to vertical transmission during the first trimester of pregnancy. This study suggests macular involvement is more strongly associated with the trimester of transmission than optic nerve changes. Because no posterior coloboma was detected, the researchers hypothesize that ZIKV does not interfere with organogenesis. At this point, it is unclear whether ocular complications in infants arise from ZIKV, microcephaly, or a combination of both. As more cases are followed, further research may elucidate the natural history of ZIKV infection and its ocular sequelae.
Ventura C, Maia M, Travassos S, et al. JAMA Ophthalmol. August 2016. 134(8): 912-918.
Optical Coherence Tomography Features of Active and Inactive Retinal Neovascularization in Proliferative Diabetic Retinopathy
The purpose of this study was to investigate the use of spectral-domain optical coherence tomography (SD-OCT) to describe features of retinal neovascularization of the disc or elsewhere (NVD or NVE) in proliferative diabetic retinopathy (PDR), to assist in recognizing signs of new vessel activity.
This was a retrospective, cross-sectional study involving 43 eyes with PDR and either NVD or NVE. NVD was described as new vessel complexes located in the disc or 1 disc-diameter from its margin, and NVE was described as new vessels growth located anywhere outside of this area. Each patient underwent a clinical exam, fundus photos, fluorescein angiography and OCT.
Five distinct features were identified to be significantly difference between active and inactive new vessel complexes. There was a high rate of vitreous hyper-reflective dots in active neovascularization; this may be due to coalesced clusters of sero-sanguinous components that are leaking from these active vessels. Inactive or quiescent neovascularization had features more suggestive of fibrotic changes, including the presence of an epiretinal membrane adjacent to the new vessels, as well as inner retinal tissue contracture and vitreous invasion. Also, inactive neovascularization was shown to protrude towards the vitreous, unlike active vessels.
In conclusion, through the use of OCT, the aforementioned differentiating clinical features may be useful in determining disease activity. Due to the non-invasive nature of OCT, more frequent imaging, than fluorescein angiography allows, may be performed to aid in decision making and monitoring response to treatment.
Vaz-Pereira, S, Zarranz-Ventura, J, Sim, D et al. Retina. June 2016 36(6):1132-1142
Implication of Recurrent or Retained Fluid on Optical Coherence Tomography for Visual Acuity During Active Treatment of Neovascular Age-Related Macular Degeneration with a Treat and Extend Protocol
The purpose of this study was to evaluate the relationship between findings on optical coherence tomography (OCT) and visual acuity in patients receiving a 12-month “treat and extend” period with anti-VEGF agent, ranibizumab.
This was a retrospective study involving 103 eyes with over a period of 12 months. Patients included in this study had to be 50 years of age or older, had to have a sub-foveal choroidal neovascular membrane (CNVM) secondary to age-related macular degeneration (documented by fluorescein angiography) and only received ranibizumab treatment. Their sole treatment was required to be a treat and extend protocol with at least a 12-month follow up.
The treat and extend protocol was as follows: intravitreal injection of 0.5mg/0.05mL ranibizumab (Lucentis) given at 3 initial monthly injections followed by treatment deemed appropriate by clinical examination, visual acuity and OCT. Those with no loss in best-corrected visual acuity (BCVA) without signs of new subretinal (SRF) or intraretinal fluid (IRF) were given an injection with an extended 2-week interval, not exceeding 12 weeks. If there was a decrease in BCVA or new SRF or IRF, 4 weekly treatments were given until resolution.
The patients in this study achieved about an 8-letter gain in visual acuity over 12 months, with an average of about 8 injections. Fluid location played a role in the prognosis of these patients. Subretinal fluid was not a major determinant of visual acuity; patients maintained similar vision. However, those with intra-retinal fluid had significantly worse vision. Interestingly, there was a better indication of visual recovery in patients with intraretinal fluid over those with subretinal fluid. The evidence of fluid, however, did not always lead to vision loss. This suggests that the location of the fluid and integrity of the outer retina may be more importance in determining a change in visual acuity. It is important to monitor the structural integrity of the outer retinal anatomy as well as changes in pigment epithelial detachments. Where fluid was persistent, there was either stable vision or only a small change of worsening vision.
In conclusion, fluid noted on OCT is not always related to a decreased in visual acuity. New onset fluid (intraretinal > subretinal) is more likely to lead to significant vision loss over those eyes that maintained persistent fluid.
Wickremasinghe,S, Janakan, V, Sandhu, S, et al. Retina. July 2016 36(7):1331-9
Subretinal Fluid Associated with MEK Inhibitor Use in the Treatment of Systemic Cancer
Studies have shown that the use mitogen-activated protein kinase (MAPK) kinase inhibitors (MEK), an emerging class of drugs in the treatment of metastatic cancer, leads to subretinal fluid (SRF) that mimics central serous chorioretinopathy (CSC). The goal of this study is to determine whether the associated SRF poses a significant threat to vision over time, and if so, should MEK therapy be modified or discontinued altogether?
Researchers performed post-hoc analysis of data collected from 51 patients enrolled in four oncology clinical trials that investigate combination therapy with binimetinib, a selective MEK1/2 inhibitor. Ophthalmic examination was performed every two weeks for 2 months after starting medication, then monthly thereafter by a retina specialist. In 90% of participants, SRF was present, with 78% showing fluid on OCT by two weeks after initiating MEK therapy. The location of SRF varied but in 63% of cases it developed both subfoveally and along the arcades. Of those patients with SRF, only 20% were symptomatic, reporting transient blurry vision or central distortion that occurred between 45 to 120 minutes after drug administration, with complete resolution of symptoms as early as two hours after onset. Snellen visual acuity remained within one line of baseline in 90% of participants. In 41% of patients, there was no detectable SRF by the last clinical exam—a median of 60 days after starting medication treatment. This demonstrates the high variability and instability of SRF in these study patients, where most individuals were asymptomatic and did not experience a change in visual acuity.
While the prevalence of binimetinib-associated SRF was high in this study, visual symptoms are uncommon and the development of SRF is highly transient. Thus, it is unlikely that the ocular risks of MEK therapy outweigh the benefits regarding survivability in the setting of advanced, metastatic cancer. As this treatment becomes more widely available, further study will be needed to assess the long-term effects of MEK inhibitors on ocular health as it relates to proper dosing and screening protocols.
Weber M, Liang M, Flaherty K, et al. JAMA Ophthalmol. August 2016. 134(8): 855-862.
Safety and Efficacy of Intravitreal Dexamethasone Implants in The Management of Macular Edema Secondary to Infectious Uveitis
The purpose of this retrospective review was to investigate the safety and efficacy of intravitreal dexamethasone implants (IDI) in the treatment of macular edema as a result of infectious uveitis.
Clinical records of 8 eyes in 7 patients treated for macular edema (central macular thickness greater than 300 microns and fluid in the macula on OCT) secondary to infectious uveitis resulting from Herpes-simplex 1, Varicella- Zoster virus, Treponema pallidum, Brucella mellitensis, Borrelia burgdorferi, Toxoplasma gondii and cytomegalovirus infections were reviewed. Prior to IDI injection, all patients had recently finished or were receiving systemic antimicrobial drugs for the infectious etiologies. Only patients with definitive diagnosis following positive microbiological test results and those followed for at least 6 months were included in the retrospective review. Resolution of macular edema, improvement in visual acuity as well as rate of reactivation of infection following treatment were assessed. The median follow-up time was 18 months.
Following intravitreal Dexamethasone implant injection, visual acuity in all eyes improved from a median BCVA of 20/160 to median BCVA of 20/70 at the last follow up visit. At baseline, central macular thickness was 516 microns and 266.3 microns at the last follow up visit, without evidence of macular edema on OCT. 6 eyes received reinjections of the implant. Two patients required vitreoretinal surgery for epiretinal membrane and rhegmatogenous retinal detachment during follow-up. However, no patients experienced an increase in intraocular pressure during the follow up period.
In conclusion, in this retrospective review the use of IDIs in patients with macular edema secondary to infectious uveitis was effective and safe. Significant improvements in visual acuity were noted with IDIs. Additionally, the mean central macular thickness decreased in all eyes and no evidence of macular edema was observed on the last follow up visit. Furthermore, IDIs did not lead to reactivation of infectious ocular disease in this small case series and can be considered as a treatment modality in macular edema secondary to infectious uveitis.
Fonollosa, A, Llorenc, V, Artaraz, J et al. Retina. September 2016. 36(9): 1778-1785
Increased Choroidal Vascularity in Central Serous Chorioretinopathy Quantified Using Swept-Source Optical Coherence Tomography
The purpose of this study was to evaluate the dilation of the choroidal vasculature that occurs in patients suffering from Central Serous Chorioretinopathy (CSC) through the use of Swept-Source Optical Coherence Tomography (SS-OCT).
40 eyes of 34 previously diagnosed CSC patients were examined during the course of this study. Using SS-OCT technology, three-dimensional images of the choroid were obtained that focused on the macular area. Images were obtained in two different size settings: 3 x 3 mm and 6 x 6 mm. Also, en face images of the microvasculature of both the inner choroid and large choroidal vessels were converted in binary images and analyzed quantitatively. Results from this study showed that the eyes diagnosed with CSC had larger choroidal vasculature areas in comparison to age-matched normal eyes. Likewise, the choroidal vascular area was larger in eyes with the multicoal posterior pigment epitheliopathy form of CSC in comparison to eyes with the classic form of CSC or the diffuse retinal pigment epitheliopathy form of CSC. Another finding was that the subfoveal thickness was strongly associated with the vascular area that was at the level of the choroidal vessels.
In conclusion, eyes diagnosed with CSC displayed an increased choroidal vascular area that included the entire macular area. Therefore, it may be suggested that CSC may be a result of a disturbance that occurs in the choroidal circulation.
Yoshimasa, K., Sotaro, O., Kenji, Y., et al. AJO. September 2016. 169: 199-207
Pseudodrusen and Incidence of Late Age-Related Macular Degeneration in Fellow Eyes in the Comparison of Age-Related Macular Degeneration Treatments Trials
The purpose of this study is to evaluate the association between pseudodrusen and incidence of late age-related macular degeneration (AMD) in fellow eyes of patients with unilateral neovascular AMD (nAMD).
This was a cohort study within the Comparison of AMD Treatment Trials (CATT), with patients (620 fellow eyes) with neither nAMD nor geographic atrophy (GA) in the fellow eye at baseline. Digital color fundus photography (CFP) viewed under full color, green channel, and blue channel; red-free images; and fluorescein angiography (FA) were used to assess the presence and type (dot, reticular, or confluent) of baseline pseudodrusen. At baseline, 176 fellow eyes (28.4%) had pseudodrusen (55% dot, 82% reticular, 35% confluent). At 2 years, nAMD occurred in 54 eyes (30.7%) with pseudodrusen and in 72 eyes (16.2%) without pseudodrusen; GA occurred in 27 eyes (15.3%) with pseudodrusen and in 37 eyes (8.3%) without pseudodrusen; late AMD occurred in 73 eyes (41.5%) with pseudodrusen and in 101 eyes (22.8%) without pseudodrusen. Dot pseudodrusen were associated independently with nAMD, while confluent pseudodrusen were associated independently with GA. Finally, eyes with pseudodrusen had increased incidence of late AMD regardless of the Age-Related Eye Diseases Study (AREDS) severity score.
The authors concluded that baseline pseudodrusen in the fellow eye of CATT participants were associated with approximately 2 times higher risk of late AMD through 2 years. Pseudodrusen were associated independently with a higher incidence of nAMD (dot pseudodrusen) and GA (confluent pseudodrusen). These findings indicate that pseudodrusen should be considered alongside the AREDS severity score for the prediction of late AMD.
Zhou, Q, Ebenezer, D, Maguire, M et al. Ophthalmology. July 2016. 123:1530-1540
A Perspective on the Nature and Frequency of Pigment Epithelial Detachments
The purpose of this prospective consecutive case series was to describe and compare the clinical and imaging characteristics of pigment epithelial detachments (PEDs) in age-related macular degeneration (AMD), polypoidal choroidal vasculopathy (PCV) and central serous chorioretinopathy (CSC). This study involved 174 eyes with PEDs. Clinical examinations as well as color fundus photos (Topcon), and spectral domain OCTs (Spectralis) were documented.
Age-related macular degeneration was the most common etiology of PEDs in this series. Drusenoid PEDs were the most non-vascularized PED subtype accounting for 41% of the patient base. Drusenoid PEDs were usually of smaller diameter and affected the central macula. Clinically they appear as yellowish-white lobular structures. On OCT, they appear as discrete lobular detachments of the RPE with underlying hyper-reflective material. One of the most important features of a drusenoid detachment is the presence of a vitelliform detachment in the subretinal space overlying the PED. Larger vascularized PEDs associated with AMD included type 1 and type 3 neovascularization (NV). Type 1 NV was characterized by central PEDs with subretinal hemorrhages and exudation. Peri-foveal PEDs with intra-retinal cysts and hemorrhages were more common in type 3 NV. Type 2 NV was not associated with a PED in this series.
Polypoidal Choroidal vasculopathy was the second most common disease associated with PEDs, affecting approximately 9% of patients. Compared to other PED subtypes in our study cohort, these were significantly larger, eccentric and vascularized; they contain polyps with multi-layer hemorrhages in patients with a normal to thick choroid. Polyps can be visualized on OCT underneath the surface of a large serous PED as a series of round structures, or as a smaller peaked PED adjacent to a larger serous PED or as sharp peak like elevations within a PED.
Central serous chorioretinopathy was the least common disease associated with PEDs and only affected about 5% of the study cohort. Acute CSC presented with serous PEDs along with areas of neurosensory detachments. Chronic CSC was defined by the presence a PED, thickened choroid and pigmentary changes but no sensory detachment. Pigment changes were suggestive of a possible previous CSC. These PEDs were smaller, multiple, eccentric, serous, non-vascularized almost always with a thick choroid and no evidence of drusen. The OCT findings of an associated serous PED typically show a well circumscribed convex, dome-shaped, out-pouching of the RPE with a smooth surface.
Awareness and understanding of the characteristic clinical and imaging features of PEDs associated with various chorioretinal degenerative diseases will assist eye care specialists in making a specific diagnosis.
Tan, A , Simhaee, D, Balaratnasingam,C, et al. American journal of ophthalmology. September 2016
Intravitreal Bevacizumab for Choroidal Neovascularization in Age-Related Macular Degeneration
5-Year Results of the Pan-American Collaborative Retina Study Group
The purpose of this retrospective case series was to report the long-term functional and structural outcomes of patients with choroidal neovascularization secondary to age related macular degeneration treated with intravitreal bevacizumab (IVB)
Clinical records of 247 patients (292 eyes) diagnosed with subfoveal choroidal neovascularization secondary to age related macular degeneration that were treated with at least one intravitreal injection of 1.25 mg of bevacizumab were reviewed. Patients over 50 years of age with decreased acuity, no other previous treatment for exudative AMD, no evidence of disciform scarring (defined as >50% subretinal fibrosis), no evidence of intraocular inflammation, no uncontrolled intraocular pressure and no cataract surgery within the past 6 months were included in the study. Patients were followed and treated monthly until resolution of subretinal and intraretinal fluid was observed. Reinjections were administered whenever recurrence (defined as decrease in BCVA, new hemorrhage in the macular area, presence of intraretinal or subretinal fluid, or CNV activity on FA) of choroidal neovascularization was noted. Snellen visual acuity testing, optical coherence tomography, fluorescein angiography and fundus examination were performed at baseline and at follow-up visits.
The 60 month BCVA analysis demonstrated 18.8% of eyes improved > 2 lines, 8.6% had a gain of > 3 lines, 45.9% remained stable but 17.8% of eye lost > 3lines of BCVA.
At the 60 months follow up, 15.4% had BCVA >20/40 while 53.8% had a BCVA <20/200.
The mean central macular thickness at each follow up was significantly decreased from baseline. Geographic atrophy was observed in 16% of eyes at baseline, but at 5 year follow up GA developed or progressed in 42.5% of eyes.
In conclusion, the early improvement in visual acuity following IVB was not maintained at 5 years of follow-up. It is difficult to determine why patients did not maintain their initial visual gains. It is unlikely that the patients were undertreated and visual loss may be attributed to development of tachyphylaxis to bevacizumab. While this study was uncontrolled, nonrandomized and retrospective, it is important to note that IVB may play a role in the development and progression of geographic atrophy in patients with subfoveal choroidal neovascular membrane secondary to AMD.
Arevalo, J, Lasave, A, Wu, L et al. Retina. May 2016. 36(5): 859-867.

|
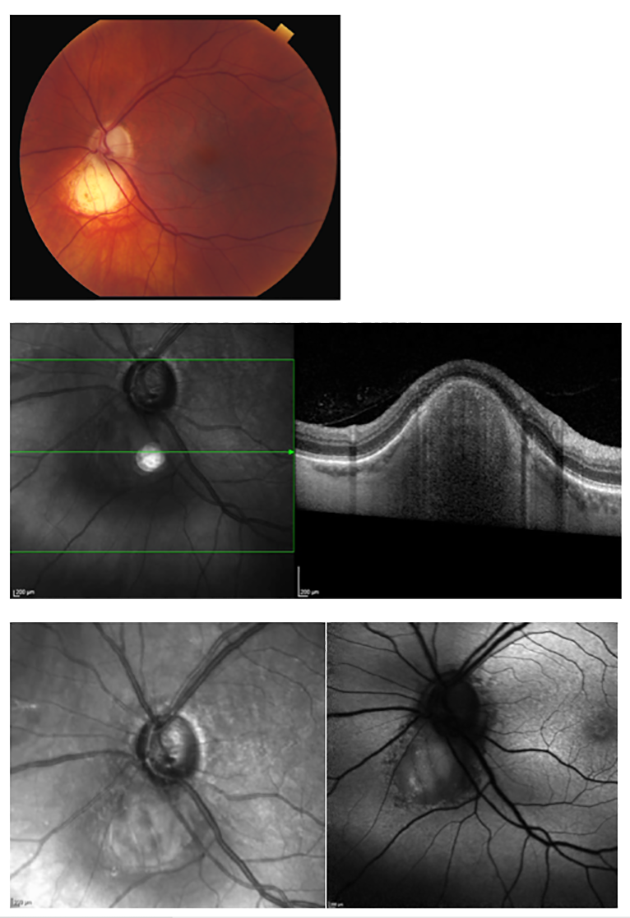
ANSWER
TO "YOU MAKE THE DIAGNOSIS"
This lesion represents solitary idiopathic choroiditis (SIC) or unifocal helioid choroiditis. SIC was first described by Hong et al in 1997, and was given its name of unifocal helioid choroiditis as a result of the lesion’s sun-like appearance. SIC occurs as a single, discrete, yellow-white choroidal lesion in the posterior pole. It is approximately one disc diameter in size, shows minimal growth, and may resemble an intraocular tumor. In its active state, the margins are less discrete with associated exudates, local hemorrhages, and overlying subretinal fluid. Choroidal neovascularization is rarely associated with the lesion. These slightly hazy borders distinguish active SIC from its inactive state. When inactive, the borders are well-defined and surrounded by an indistinct red-orange halo. The condition is often self-limiting although relapses may occur. It starts as a discrete area of focal choroiditis and evolves into a chronic lesion with resolution of the overlying subretinal fluid and some decrease in thickness. Once the lesion is no longer active and the patient is asymptomatic, periodic observation is sufficient management. If an active lesion is near the fovea and poses a risk to vision, however, a short course of oral steroids is often prescribed. In a few patients with associated subretinal hemorrhage, anti-VEGF injections have been used with some success.
There is no demographic predilection, although most patients have been Caucasian and young to middle-aged at the time of diagnosis. As with the patient in this case study, most patients are asymptomatic, unless the location of the lesion and/or associated fluid is affecting visual acuity. Otherwise, there are usually no signs of anterior or posterior inflammation and no subjective complaints by the patient.
Evident by the lesion’s description as solitary idiopathic choroiditis, the condition has no specific etiology. Extensive laboratory and radiological testing, as well as ancillary ophthalmic testing, does not indicate a specific cause for the lesion. However, one case report has suggested a link between SIC and coxsackie virus, and others have indicated the lesion as a possible manifestation of cat-scratch disease. As SIC can be confused with more concerning intraocular lesions, auxiliary testing is important to help distinguish SIC from its differentials, such as amelanotic nevi, choroidal metastasis, choroidal osteomas, choroidal hemangiomas, sclerochoroidal calcifications, and choroidal granulomas from infectious conditions such as toxoplasmosis or tuberculosis , to name a few. After ruling out these other conditions, these lesions can be monitored routinely, with serial photos as an aid, to look for any active issues as stated above.
Steven Ferrucci, OD, FAAO, ORS Fellow and Vice President, ORS
Joann Choi, OD, Optometric Resident, Sepulveda VA |

IN THE
NEWS
 |
Eylea, Lucentis less cost-effective than Avastin for treatment of DME
Aflibercept and ranibizumab were less cost-effective than bevacizumab in the treatment of diabetic macular edema, according to a post hoc analysis of data from the Diabetic Retinopathy Clinical Research Network Protocol T tria, according to a recent study In JAMA Ophthalmology.
The analysis included 624 patients randomized to Eylea (aflibercept, Regeneron), Avastin (bevacizumab, Genentech) or Lucentis (ranibizumab, Genentech).
Based on 2015 wholesale acquisition costs, the cost of aflibercept 2 mg was $1,850, ranibizumab 0.3 mg $1,170 and repackaged 1.25 mg bevacizumab about $60 per dose.
Investigators calculated incremental cost-effectiveness ratios (ICERs) for aflibercept, bevacizumab and ranibizumab for 1 year and then projected 10-year results. ICERs were calculated for participants and subgroups with baseline visual acuity of 20/32 to 20/40 and 20/50 or worse.
Over 1 year for all patients, the ICER of aflibercept compared with bevacizumab was $1.11 million per quality-adjusted life-year (QALY), and the ICER of ranibizumab compared with bevacizumab was $1.73 million per QALY.
Over 10 years for all patients, the ICER of aflibercept compared with bevacizumab was $349,000 per QALY, and the ICER of ranibizumab compared with bevacizumab was $603,000 per QALY.
In eyes with decreased vision from DME, treatment costs of aflibercept and ranibizumab would need to decrease by 69% and 80%, respectively, to reach a cost-effectiveness threshold of $100,000 per QALY compared with bevacizumab during a 10-year horizon; for the subgroup with worse baseline vision, the costs would need to decrease by 62% and 84%, respectively, the study concluded.
|
 |
FDA approves Humira for treatment of noninfectious intermediate, posterior and panuveitis
The FDA has approved Humira for the treatment of noninfectious intermediate and posterior uveitis and panuveitis, according to a press release from AbbVie.
With this approval, the company now has 10 approved indications for Humira (adalimumab) in the U.S. for immune-mediated diseases.
In June, the European Commission approved Humira for the treatment of noninfectious intermediate and posterior uveitis and panuveitis. In the U.S., this is the first non-corticosteroid treatment available for these indications.
The approval was based on the phase 3 VISUAL-I and VISUAL-II studies, which showed adult patients with noninfectious intermediate and posterior uveitis and panuveitis treated with Humira had a significantly lower risk of uveitic flare and decreased visual acuity compared with placebo.
|
 |
AAO revises screening guidelines for chloroquine, hydroxychloroquine retinopathy
The American Academy of Ophthalmology revised its recommendations on screening for chloroquine and hydroxychloroquine retinopathy based on new information about the prevalence of toxicity, risk factors, fundus distribution and effectiveness of screening tools, according to a recent study in Ophthalmology by Dr. Marmor and colleagues..
The AAO recommends a maximum daily hydroxychloroquine use of 5.0 mg/kg real weight. While researchers assured there are no similar demographic data for chloroquine, dose comparisons in previous data suggest using 2.3 mg/kg real weight.
Toxicity risk is dependent on daily dose and duration of use, according to researchers.
Using the recommended doses, the risk of toxicity up to 5 years is under 1% and up to 10 years is less than 2%, but rises to almost 20% after 20 years.
The AAO recommends a baseline fundus examination to rule out preexisting maculopathy.
Annual screening should begin after 5 years for patients on acceptable doses without major risk factors, said researchers.
The risk of vision loss is minimal if retinopathy was detected early, but significant if a bull’s eye lesion and some reduction in central foveal thickness are present, as damage can progress for a number of years, according to researchers.
|
 |
OASIS trial: Ocriplasmin improves VMA resolution over long term
Ocriplasmin improved resolution of symptomatic vitreomacular adhesion, according to 2-year results of the OASIS trial.
The phase 3b randomized, sham-controlled, double-masked, multicenter clinical trial included 220 patients; 146 patients received intravitreal Jetrea 0.125 mg (ocriplasmin, ThromboGenics), and 74 patients received a sham injection. Patients were evaluated at 12 visits over 24 months.
The primary efficacy endpoint was the proportion of subjects with pharmacologic resolution of VMA at 28 days. Secondary efficacy endpoints, assessed at 24 months, included the proportion of patients who gained best corrected visual acuity from baseline, experienced nonsurgical full-thickness macular hole closure and underwent vitrectomy, in addition to Visual Function Questionnaire scores.
The primary endpoint was achieved, with a VMA resolution rate of 41.7% in the ocriplasmin group and 6.2% in the sham group at 28 days. The between-group difference was statistically significant (P < .001). The treatment effect continued throughout the study period.
A two-line or greater improvement in BCVA was seen in 50.5% of patients in the ocriplasmin group and 39.1% of those in the sham injection group. Nonsurgical full-thickness macular hole closure was achieved in 30% of eyes in the ocriplasmin group and 15.4% of eyes in the sham group. Neither of these between-group differences were statistically significant.
Vitrectomy was performed in 33% of patients in the ocriplasmin group and 43% of those in the sham group (P = .08). VFQ-25 scores improved by five points or more from baseline, regardless of vitrectomy, in 51.4% of patients in the ocriplasmin group and 30.1% of those in the sham group (P = .003)
Adverse events tended to be mild to moderate and transient, with a short onset time.
|
 |
TANZANITE study: No re-treatments required with triamcinolone acetonide formulation after 3 months
A majority of patients treated with a proprietary form of triamcinolone acetonide in combination with aflibercept required no additional treatments over 3 months compared with patients treated with aflibercept alone, Clearside Biomedical announced in a press release.
The phase 2 TANZANITE clinical trial included 46 treatment-naïve patients with macular edema associated with retinal vein occlusion who were randomized to receive suprachoroidally administered Zuprata (triamcinolone acetonide, Clearside) in combination with intravitreally administered Eylea (aflibercept, Regeneron) or Eylea alone.
Eighteen of 23 patients (78%) in the active arm required no additional treatments over 3 months compared with seven of 23 patients (30%) in the control arm (P = .003).
The primary endpoint of reducing the need for aflibercept re-treatments was announced in April; preliminary results showed that approximately 60% fewer aflibercept injections were required in the active arm than in the control arm (P = .013).
The study also met secondary endpoints of mean change from baseline in best corrected visual acuity and central subfield thickness. At 3 months, the active arm had a mean improvement of 19 letters compared with 11 letters in the control arm.
Clearside plans to have an end of phase 2 meeting with the FDA in the second half of the year, and if feedback from the FDA is positive, the company intends to initiate a phase 3 clinical trial in the first half of 2017, the release said.
|
 |
Early data ‘promising’ for gene therapy for Leber’s hereditary optic neuropathy
GenSight Biologics reported “promising” preliminary data on its gene therapy product for the treatment of neurodegenerative retinal disease, according to a press release.
The study included 15 patients with Leber’s hereditary optic neuropathy (LHON) grouped into five groups, with each group of three patients receiving an escalating dose of GS010 via single intravitreal injection in the more severely affected eye. Mean onset of disease was 6 years. Enrollment in the phase 1/2 safety and tolerability study was completed in April 2015.
At 48 weeks after injection, patients with disease onset of less than 2 years gained an average of 30 letters in the treated eye and 13 letters in the untreated eye, according to the release. In patients with disease onset of more than 2 years, there was no significant difference in letter gain between eyes.
According to the release, the GS010 uses mitochondrial targeting sequence technology and an adeno-associated virus vector to address defects inside mitochondria.
|
 |
Certain diabetic retinopathy stages associated with higher levels of depression
The association between depressive symptoms, diabetes and diabetic retinopathy is likely to be bidirectional, with diabetes impairment complicating depression and vice versa, according to a study in JAMA Ophthalmology.
The cross-sectional study included 519 patients with diabetes, of which 170 individuals (32.8%) were female. Average patient age was 64.9 years.
Researchers utilized the Hospital Anxiety and Depression Scale to measure depression and anxiety symptoms; scores range from 0 to 21, and scores over 8 signify possible anxiety or depression, according to researchers.
A total of 80 individuals (15.4%) screened positive for depressive symptoms, and 118 patients (22.7%) screened positive for symptoms of anxiety.
Diabetic macular edema was not associated with depressive symptoms.
Researchers found that severe nonproliferative diabetic retinopathy (NPDR)/PDR was independently associated with greater depressive symptoms after accounting for sociodemographics and clinical characteristics, including visual acuity.
Furthermore, researchers concluded that a self-reported history of anxiety or depression, longer duration of diabetes, more severe diabetic retinopathy, poorer blood glucose control, lower educational level and severe vision impairment were associated with greater depressive symptoms.
Greater symptoms of anxiety were associated with self-reported history of anxiety or depression, presence of comorbidity, younger age, lower educational level and female sex, according to researchers.
|
 |
Mark Humayun, MD, PhD, receives National Medal of Technology and Innovation for Argus II research
Mark S. Humayun, MD, PhD, received the National Medal of Technology and Innovation from President Barack Obama on May 19, according to the American Academy of Ophthalmology.
Humayun, of USC Roski Eye Institute, was recognized for his role in developing the Argus II retinal prosthesis (Second Sight), which restores functional vision in patients with retinitis pigmentosa.
“Dr. Mark Humayun is a gifted clinician and a profoundly impactful investigator. His sustained pursuit of one of the holy grails of ophthalmology — to generate a sense of vision where none naturally exists — has changed forever our options in managing some forms of retinal blindness,” David W. Parke II, MD, CEO of the AAO, said in a statement. “The profession is proud of his accomplishments and delighted that they have been nationally recognized and celebrated.”
The Argus II implant is approved by the FDA and has CE mark designation in Europe. It is currently being investigated in the treatment of age-related macular degeneration.
Humayun and colleagues published a study in Ophthalmology in August 2015 showing that 29 of 30 patients had functioning Argus II systems 3 years after implantation. Overall, the device improved visual function.
The National Medal of Technology and Innovation was created in 1980 and recognizes individuals who make enduring contributions to U.S. competitiveness and quality of life and contribute to the country’s technological workforce.
|
 |
Oral bisphosphonates associated with increased risk of wet AMD
People who use oral bisphosphonates may have an increased risk of developing wet age-related macular degeneration, according to a study.
Investigators used three study designs: disproportionality analysis, case-control study and self-controlled case series. They gathered data from the FDA Adverse Event Reporting System database and data from two patient cohorts in British Columbia.
The disproportionality analysis showed 58 cases of AMD reported with alendronate, 17 cases with ibandronate and 11 with risedronate. The reported odds ratios were 3.82 with alendronate, 2.40 with ibandronate and 2.87 with risedronate.
The case-control analysis included 6,367 patients with AMD. The adjusted odds ratios for patients with 3 years of exposure to oral bisphosphonates were 1.24 at 1 year, 1.38 at 2 years and 1.59 at 3 years.
The self-controlled case series included 193 cases of wet AMD on continuous bisphosphonate use. The risk ratios for AMD were 1.22 at 1 year and 1.87 at 5 years.
|
 |
Fatty acids from oily fish may reduce sight-threatening DR risk in older patients with diabetes
Regular intake of long-chain omega-3 polyunsaturated fatty acids obtained from oily fish was associated with a reduced risk of sight-threatening diabetic retinopathy in middle-aged and older patients with type 2 diabetes, according to a study conducted in Spain.
The study’s finding that consumption of at least 500 mg/d of dietary long-chain omega-3 polyunsaturated fatty acids (LC3PUFAs) decreased the risk of diabetic retinopathy (DR) in patients with diabetes corroborates experimental models and the current theory of DR pathogenesis, according to the report.
The prospective investigation included 3,482 patients with a mean age of 67 years diagnosed with type 2 diabetes who had participated in the PREDIMED study, a randomized clinical trial that tested Mediterranean diets supplemented with extra virgin olive oil or nuts vs. a control diet for primary cardiovascular prevention.
Among the 3,482 patients, 2,611 (75%) consumed the recommended amount of at least 500 mg/d of LC3PUFA, which could be achieved with two servings of oily fish per week.
The primary outcome measure was incident DR requiring laser photocoagulation, vitrectomy and/or antiangiogenic therapy. Median follow-up was 6 years. Sixty-nine new events were recorded during this time.
Adjusted data showed that patients who met the recommendation of at least 500 mg/d of LC3PUFA had a 48% reduced risk of incident sight-threatening DR compared with patients who consumed less than 500 mg/d. The difference was statistically significant (P = .001).
The risk was reduced further in patients with hypertension, diabetes duration more than 5 years and insulin therapy at baseline.
Patients who did not meet the recommended LC3PUFA intake were older, smoked less, had a higher prevalence of hypertension and were treated with insulin more frequently than those who met the recommendation
|

MEET
THE FELLOWS
In each issue, a Fellow of the Optometric Retinal Society is highlighted. In this issue, Dr. Jay Haynie, a new ORS fellow, will be highlighted.
Dr. Jay M. Haynie is the Executive Clinical Director of Retina and Macula Specialists with offices in Washington State. He graduated from Pacific University College of Optometry and completed a residency at American Lake Veterans Hospital in Tacoma, WA. He has been a clinical investigator for Rainier Research and involved in several clinical studies as a sub-investigator. He serves as adjunct assistant Professor at Pacific University College of Optometry in addition to directing an internship for 4th year Optometry students. He is a Fellow of the American Academy of Optometry and a Fellow of the Optometric Retina Society. He is a published author and has become a nationally recognized speaker on new technology and treatment of retina and macular disease.
In his free time he enjoys travelling with his family, attending college football and basketball games, and if time permits taking in a round of golf. He and his wife (and best friend) Kelly are patiently awaiting grandchildren however nothing is coming soon is what they hear from their children.....
|
Revised Guidelines on Screening for Chloroquine and Hydroxychloroquine
Diana Shechtman, OD, FAAO,
Sherrol Reynolds, OD, FAAO and Steven Ferrucci, OD, FAAO
Recently, the American Academy of Ophthalmology released their 2016 revised recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy. Hydroxychloroquine (plaquenil) and the seldom used chloroquine are medications first used as anti-malarias but have become widely used for patients with rheumatologic disorders such as RA, lupus and similar conditions. These medications have been associated with causing macular toxicity, classically appearing as “bulls- eye maculopathy”. Although the incidence is relatively low, in 2011 the AAO recommended screening with newer diagnostic agents, and have recently revised the initial recommendations. They recommend.
Baseline Screening
Fundus examination within first year of use
Add visual fields and SD-OCT if maculopathy is present
Annual Screening
Begin after 5 years of use
Sooner in the presence of major risk factors
These include doses higher than 5.0 mg/kg of real weight, concurrent kidney disease , or tamoxifen use
FAF and mf-ERG can be sued in conjunction with rutile exams and SD-OCT to detect any retinopathy before it is visible in the fundus.
If definitive signs of retinopathy are determined, a decision to stop the medication should be made in conjunction with the prescribing medical physician.
(Marmor ME, et al. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revison) Ophthalmology 2016; 123:1386-1394. )
|
WHY
BECOME AN ORS FELLOW?
By Bill Denton, O.D., F.A.A.O.
Chair, Membership Committee
At some point in your career, you realize you just may be coasting. Your knowledge has been limited to the journals you receive and attempt to read, and the conferences that may not be as fulfilling as they once were. You simply need a challenge that will add an extra dimension to your professional learning.
Fellowship in the Optometric Retina Society (ORS) can provide several benefits in addition to the initial challenge of qualifying for this honor. Plenty of perks accompany your induction, but the coolest part is being associated with a body of knowledge and resources which can help you in many other ways. It is not uncommon to receive weekly thought-provoking emails about challenging cases and treatment dilemmas. Some fellows like to share their awesome cases they have diagnosed, while others post their cases with hopes that other Fellows will suggest an alternative differential diagnosis. At times it is like a round-table of brainstorming, but through the use of modern technology. Fellowship has little obligation with a huge opportunity for professional growth.
If you are up to the challenge of becoming a Fellow of the ORS, feel free to peruse the details and application at www.optometricretinasociety.org. Advice can be given to assist you in your quest. Feel free to contact us. |

SPONSOR NEWS

Editor
in Chief
Steven Ferrucci, OD, FAAO
Co-Editor
Mark T. Dunbar, OD, FAAO |
Journal
Reviewers
Celina Diego, OD
Tea Avdic, OD
Steve Quan, OD
Angela Diamantakos, OD
Faten Edriskhalaf, OD
Jenna Blechman, OD
Senior Graphic Designer
Matt Egger
|
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|