| |
Volume 12, Number 4 |
December
2016 |
|
|
Inside
This Issue |
|
|
|
|
|
This e-newsletter is provided free to doctors through industry support from |
 |
| |
FROM
THE DESK OF THE EDITOR
I just returned from the ORS meeting, Retina Update 2016, in Scottsdale AZ. It was a great conference , with well over 120 ODs joining us at the beautiful Westin Kierland Resort and Spa. Many ORS fellows as well as some guest lecturers provided over 12 hours of top-notch education. On Friday night, we held our first hands-on workshop with a variety of equipment that the OD could learn on and try, as well as interact with a few ORS fellows to help understand how to use these instruments and what information is being seen. A few of the other highlights of the meeting included the first lecture of the weekend, a panel discussion entitled “What Would Larry Do”, a tribute to our beloved colleague, Dr. Larry Alexander, who was so instrumental and influential in many of our careers, mine included. Another highlight was a panel discussion “Co-Management in the ICD-10 era” with Drs. Joe Pizzimenti, John Rumpakis, and Pravin Dugel, MD. This course discussed cases that were effectively co-managed between ODs and MDs, and tips on appropriate billing and coding in order to remain in compliance and profitable.
LIVE
POLL
|
How do you classify AMD in your practice?
|
|
However, for me, the highlight was the solo lecture provided by Dr. Pravin Dugel, a well-known and respected retinal specialist in the Phoenix area. He discussed the unmet need in both neovascular AMD and diabetes, and the challenges we face as eye care providers as well as a society moving forward. This might be one of the most informative and thought-provoking lectures I have ever attended, as he presented many issues regarding the future of retinal treatment, the future of anti-VEGF injections, and the moral and financial responsibilities that must be discussed as new therapies become available for retinal disease.
I really want to thank my ORS fellows, who have honestly become some of my closest colleagues and friends within optometry. A special thanks to Joe Pizzimenti, and Brad Sutton as educational co-chairs for selecting and developing a great series of lectures. Thanks to Mo Rafieertary (who thinks he is my only friend) as our industry relations chair for getting several exhibitors to help sponsor our meeting. And thanks to those sponsors, Annidis, Centervue, Diopsys, EyePromise, Heidleberg, MacuHealth, Optovue, Topcon, and Zeiss, without whom holding such a meeting would not be possible.
I also want to thank Review of Optometry and their staff, particularly Jonathan Dardine, Mike Hoster, Margaret DiColli, and Casey Foster, for helping to administer and run the meeting. Without their help, we would be lost.
Lastly I want to thank all the ODs who chose to take time and spend the weekend with us. I truly hope you felt our meeting was education, entertaining and worthwhile, and provided insights you can use in your practice to better the care of your patients with retinal disease.
Steven Ferrucci, O.D., F.A.A.O.
Editor in Chief
 |
PRESIDENT'S MESSAGE
As my two-year cycle of being the President of the ORS comes to a close,
OCTOBER 2016
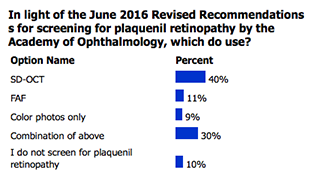
POLL RESULTS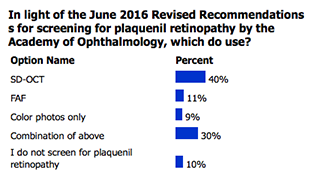
|
I am truly grateful for the opportunity that my colleagues in the organization have given me. I am grateful for the groundwork laid by past ORS Presidents such as Joe Pizzimenti, Bill Jones, Jerome Sherman, and of course the late Larry Alexander. To be sure, this “volunteer” position has added quite a bit to an already full plate. That having been said, I would not trade these past two years for anything. I have strengthened and enhanced many pre-existing friendships with other ORS Fellows, and forged many new relationships as well. I have had the good fortune of working very closely with some very energetic and highly skilled individuals at Jobson Publishing to put on our yearly ORS continuing education conference. I am not going to list names, because assuredly I would inadvertently leave some very deserving individuals off the list. Suffice it to say that without their dedication and hard work in this partnership, the ORS would be unable to effectively host meetings. At the end of the day, that is why we exist. To educate practitioners in the area of vitreoretinal disease, thus enabling them to have a positive impact on the lives of their patients. The next President’s message will come from a new leader, who I am certain will continue the legacy of advancing both our organization and the profession that we all love. I will always cherish having been given the opportunity to do just that.
Sincerely,
Brad Sutton, OD, FAAO
President, ORS

YOU
MAKE THE DIAGNOSIS
Answer appears later in newsletter.

CLINICAL
PEARLS
Beckman Classification of AMD
By: Steven Ferrucci, OD, FAAO
ORS Fellow
In 2013, 26 AMD experts, 1 neuro-ophthalmologist, 2 committee chairmen, and 1 methodologist came up with a clinical classification system for age-related macular degeneration (AMD), called the Beckman Classification of AMD. Their goal was to devise a clinically useful classification system and common terminology for AMD that combines scientific literature and expert opinion.
Using a modified Delphi technique, they proposed a 5 stage AMD classification system.
1. No apparent aging changes : No drusen and no AMD pigmentary abnormalities
2. Normal aging changes: Only drupelets (small drusen ≤ 63µm) and no AMD pigmentary abnormalities
3. Early AMD: Medium drusen ( >63 µm and ≤ 125µm) and no AMD pigmentary abnormalities
4. Intermediate AMD: 1 Large drusen (> 125 µm) and/or any AMD pigmentary abnormalities
5. Late AMD: Neovascular AMD and/or any geographic atrophy
While not currently as widely accepted as the AREDS or AREDS simplified scale, this system appears quite easy to adapt clinically, and is gaining more traction among eye care providers. Further, its seems to be of value in predicting AMD Risk.
Ferris et al. Ophthalmology. 2013; 120 (4):844-851.
Hemorrhagic Occlusive Retinal Vasculitis (HORV)
Maynard L. Pohl, OD, FAAO
Founding ORS Fellow
Hemorrhagic Occlusive Retinal Vasculitis, or HORV, is a newly- identified retinopathy characterized by delayed-onset of severe vision loss ranging from 20/200 to NLP, moderate anterior chamber and vitreous inflammation, sectoral or large and confluent hemorrhage in a non-perfused retina, and peripheral and macular ischemia in the advanced stages leading to neovascular glaucoma. Reasearchers have determined that the rare although severe vasculitis affecting the venules and leading to blindness probably is related to type 3 hypersensitivity to vancomycin associated with cataract surgery and either intravitreal or intracameral injection or through the irrigation bottle. Similar manifestation also has been reported following vitrectomy and vancomycin treatment in patients with infectious endophthalmitis. Treatment includes aggressive intravitreal and systemic corticosteroids, early use of anti-VEGFs and panretinal photocoagulation.
American Society of Retinal Specialists (ASRS) August 2016 Annual Meeting |

JOURNAL
ABSTRACTS
LOSS OF EXTERNAL LIMITING MEMBRANE INTEGRITY PREDICTS PROGRESSION OF HYDROXYCHLOROQUINE RETINAL TOXICITY AFTER DRUG DISCONTINUATION
It has recently been shown that hydroxychloroquine (HCQ) retinopathy primarily involves the photoreceptors, and that limited progression occurs if medication is discontinued before advanced toxicity and damage of the retinal pigment epithelium occurs. The purpose of this study is to quantify the external limiting membrane (ELM) disruption and photoreceptor volume over time by using SD-OCT in eyes with HCQ toxic effects after discontinuation of the medication.
This was a retrospective chart review of patients who were screened for toxic effects of HCQ between January 1, 2009 and August 31, 2014. 10 patients were diagnosed has having HCQ retinal toxicity. Patients were excluded if they had other maculopathies, vitreomacular traction, or recent eye surgery in the past 6 months. SD-OCT images (using the Spectralis HRA+OCT device) were evaluated at baseline, intermediate and final follow-up. Measurements included the ratio of intact ELM length/Bruch membrane length, the 2-dimensional photoreceptor area between the intact ELM and Bruch membrane, and the total volume of photoreceptors.
Of 10 patients, 19 eyes were included. The mean cumulative dose of HCQ was 1,951 grams. The mean follow-up duration was 34.1 months. 12 eyes showed severe ELM disruption and 7 had intact ELM. All 19 eyes had visual defect sings of toxicity at baseline. 7 of the 12 eyes with ELM disruption had progressive ELM changes (including photoreceptor volume decline). All 7 eyes with intact ELM remained stable.
In conclusion, the status of the ELM when HCQ is discontinued can be considered an important indicator of prognosis for retinopathy. This OCT finding can be used in addition to other findings such as RPE damage and the integrity of the foveal IS/OS junction. Future evaluation, with a larger group of eyes, will help to validate these findings further.
Scarinci, F, Shaarawy, A, Narala, R, et al. Retina. October 2016. 36(10):1951-1957
Correlation of Spectral-Domain Optical Coherence Tomography Angiography and Clinical Activity in Neovascular Age Related Macular Degeneration
The purpose of this observational retrospective study was to characterize features of choroidal neovascularization in neovascular age related macular degeneration with spectral domain OCTA and to determine whether OCTA can be used to determine clinical activity of CNV.
Forty-five eyes of 35 white patients diagnosed with neovascular AMD and imaged with OCTA were included in this study. Subjects underwent medical record review for signs of clinical activity. Clinical activity was defined as the presence of one of the following: 1.new diagnosis of neovascular AMD with leakage on FA and/or the presence of fluid on OCT, 2. vision loss greater than or equal to 1 snellen line of acuity, 3.presence of new hemorrhage on fundus exam, 4.recurrent intra retinal or sub retinal fluid on structural OCT B scans, 5.presistent or increase irf or srf on structural OCT despite treatment or 6.leakage on FA. Two independent readers evaluated all OCTA images to define the presence and characteristics of CNV vessels seen in the outer retina and sub-RPE space. The OCTA were assessed for features of CNV: well or poorly circumscribed, associated fluid, presence of feeder vessel into CNV.
Clinical activity which correlated with leakage on FA and fluid on OCT B-scan in all patients was used to calculate the sensitivity and specificity of OCTA in visualizing CNV. The sensitivity of detecting CNV on a clinically active patient was 66.7% while the specificity was 100%. This study demonstrated a significant correlation between the presence of CNV on OCTA and clinical activity of CNV at the time of imaging in patients with neovascular age related macular degeneration.
Compared to FA, OCTA is a fast and non-invasive technique. While OCTA does not demonstrate leakage, it allows correlation between CNV vessels and associated fluid on the corresponding OCT B-scans. It also allows for better visualization of vascular details and in the future patients who appear clinically inactive but have CNV on OCTA may be treated. Additionally, the visualization of vascular detail such as feeder vessels, provided by the OCTA may give insight into the pathogenesis of neovascular age related macular degeneration.
Liang M, DeCarlo, T, Baumal, C et al. Retina. December 2016. 36(12): 2265-2273.
DEGRADATION OF CONTRAST SENSITIVITY FUNCTION FOLLOWING POSTERIOR VITREOUS DETACHMENT
It has been hypothesized that a posterior vitreous detachment (PVD) may reduce the contrast sensitivity function (CSF) in otherwise normal eyes. This study set out to evaluate the effects that a PVD can have on CSF.
This was a prospective observational case series involving 28 eyes from one single clinical practice. The main outcome measured was CSF. Those with normal CSF and the absence of a PVD at the study entry were included, with a subsequent development of a PVD in only one eye. The PVD was confirmed with b-scan ultrasonography. CSF was tested using the Freiburg Acuity Contrast Test (FrACT). This test operates on LED computer display. Surgery was offered to those who could not cope with the symptoms of the PVD. The surgery performed was a sutureless 25 G vitrectomy.
At the study entry, there was no noticeable difference in CSF between the two eyes of the patients included in this study. After the development of a PVD, there was a significant reduction in CSF in each of the affected eyes. There was, on average, about a 50% reduction in CSF. Of note, the patients who elected to have surgery were the ones with a higher reduction in CSF compared to others in the study. It has been noted in previous studies that the CSF will normalize following a vitrectomy. In this study, at the 1-month post-operative visit, there was about a 43% improvement in CSF. At the 12-month post-operative visit, there was about a 50% improvement in CSF, which was nearly identical to that of the control eye.
In conclusion, PVDs can be associated with significant reduction in CSF. The CSF is an important component of the visual system that may be overlooked. Although many patients can adapt to the symptoms associated with a PVD, sometimes it can have a significant impact on a patient’s quality of life.
Garcia, Giancarlo A. et al. American Journal of Ophthalmology. December 2016 172:7–12
Choriocapillaris Nonperfusion is Associated With Poor Visual Acuity in Eyes With Reticular Pseudodrusen
Investigators studied choriocapillaris blood flow in age-related macular degeneration (AMD) using optical coherence tomography angiography (OCTA) to assess visual acuity in eyes with reticular pseudodrusen (RPD) versus those with drusen alone. RPD is characterized by a yellowish reticular pattern in the macula marked by hypo-reflective lesions surrounded by hyper-reflective areas on infrared and auto-fluorescent filters.
This cross-sectional study included 29 eyes with RPD and 21 eyes of age-matched AMD patients with drusen. Eyes with late AMD (AREDS grade 4), choroidal neovascularization, geographic atrophy, myopia greater than -2.00 diopters, significant cataracts, and/or a history of surgery or intravitreal injection were excluded from study.
To quantify the nature of blood flow in the macula, the investigators defined non-perfusion as “percent choriocapillaris area of nonperfusion” (PCAN): the number of pixels that fall below a global threshold divided by the total number of pixels in the image. Nonperfusion may be the result of decreased blood flow velocity, number of blood vessels per unit area, and/or vessel caliber.
This study found that larger values of PCAN were associated with decreased visual acuity. Patients with RPD had significantly greater PCAN compared to those with drusen alone (7.31% and 3.88%, respectively; P < .001). This suggests that RPD is associated with larger areas of nonperfusion at the level of choriocapillaris and may explain the visual decline in RPD patients, who often experience visual symptoms earlier than their AMD counterparts. The authors hypothesize that RPD begins with choriocapillaris closure, followed by RPE hypoxia and irregular metabolism, leading to the accumulation of drusenoid deposits and subsequent photoreceptor degradation.
Nesper P, Soetikno B, and Fawzi A. American Journal of Ophthalmology, Feb 2017. 174: 42-55.
PATTERNS OF FUNDUS AUTOFLUORESCENCE DEFECTS IN NEOVASCULAR AGE-RELATED MACULAR DEGENERATION SUBTYPES
The purpose of this study was to describe characteristic fundus autofluorescence (FAF) patterns of different exudative age-related macular degeneration (AMD) subtypes.
This was a cross-sectional study including 52 patients from the retina service at the University of Louisville with choroidal neovascularization due to three different subtypes of AMD, including polypoidal choroidal vasculopathy (PCV), retinal angiomatous proliferation (RAP) and patients with typical neovascular AMD. Patients excluded from this study included those who were less than 50 years of age, had other retinal diseases (ie. Diabetic retinopathy, pathological myopia, angioid streaks, etc.), had previous retina laser or photodynamic therapy, or previous ocular surgery (except for cataract extraction). All patients had FAF, color fundus photos, FA, ICGA and OCT performed. The presence, location and characteristics of the FAF patterns were assessed by two retinal specialists.
Seventeen eyes with PCV, 16 eyes with RAP and 19 eyes with typical AMD were included in this study. Each of these eyes showed the same type of hyper/hypoautoflurescence patterns in the macula. Thus, there was no characteristic FAF pattern in the macula to distinguish between the three conditions listed above (PCV, RAP and typical neovascular AMD). However, there was a noticeable predominance of peripapillary FAF defects in those patients with PCV. It is hypothesized that these peripapillary defects may arise from mechanical stress caused by prominent anterior protrusion of RPE layer overlying the polypoidal vascular lesions.
In conclusion, FAF is a cost-effective, non-invasive way to easily view various aspect of the retinal structures. It is a useful tool in helping to identify PCV from other forms of neovascular AMD. The existence of peripapillary FAF defects in neovascular age-related macular degeneration maybe suggestive of polypoidal choroidal vasculopathy as a variant of neovascular age-related macular degeneration.
Ozkok, A, Sigford, D., Tezel, T. Retina. November 2016 36(11): 2191-2196
Formation of an Intraretinal Fluid Barrier in Cavitary Optic Disc Maculopathy
The authors investigated the utility of laser photocoagulation in combination with vitrectomy and gas tamponade when treating cavitary optic disc maculopathy. The rationale for such treatment is to create an intraretinal barrier to fluid migration, which presumably develops from fluctuating pressure gradients along anomalous communications between the optic nerve head and adjacent retina. It has been reported that over 50% of eyes with cavitary disc anomalies form serous maculopathy.
This is a retrospective interventional case series of 22 patients evaluated at the University of Michigan between 1991 and 2014. Half of these patients were included in the study and underwent laser photocoagulation, followed by vitrectomy and gas tamponade, with an average follow-up of 48.2 months. All patients had complete resolution of macular fluid in an average period of 8.5 months, where one patient had recurrence 14 months post-operatively, and 2 patients required multiple procedures to achieve resolution. The average pre-operative visual acuity was 20/125, which improved to a mean of 20/57 post-operatively.
To avoid injury to the papillomacular nerve fiber layer, red wavelength (647nm) laser was carefully applied in a curvilinear fashion along the temporal juxtapapillary region. No attempts were made to peel glial tissue. Patients were instructed to maintain face-down positioning at least 10 days post-operatively.
Given prior evidence that cavitary disc maculopathy generally resolves following vitrectomy alone, in conjunction with the small risk of injury due to laser application, laser photocoagulation should be reserved for cases of recurrent macular fluid or failure to vitrectomy alone. In that same vein, laser treatment should not be used prophylactically in optic disc pits without maculopathy. Although this study has a small sample size and bears no control group, it still offers a viable, alternative treatment for recalcitrant cases where evidence on successful treatment remains elusive.
Kiang L and Johnson M. American Journal of Ophthalmology. Jan 2017. 173: 34-44.
Choroidal Thickness Changes After Intravitreal Dexamethasone Implant Injection for the Treatment of Macular Edema due to Retinal Vein Occlusion
The purpose of this retrospective study was to investigate the changes in choroidal thickness and structure following intravitreal injection of a dexamethasone implant for the treatment of macular edema due to retinal vein occlusion.
Thirty one eyes of 31 patients that were treated with a single dose of dexamethasone implant for macular edema secondary to a retinal vein occlusion (RVO) were included in the study. Aside from a complete ophthalmological examination, each subject had a fluorescein angiography and OCT which were repeated at each follow up visit scheduled at 1 month, 3 months and 5 months. Eyes with increase in foveal thickness (> than 100 microns) and a decrease in one or more lines of acuity were reinjected with the dexamethasone implant at the month 5 follow up. 45.2% of subjects presented with nonischemic RVOs while 54.8% of the eyes were ischemic with the unaffected contralateral eye serving as the control. Subjects with bilateral retinal vein occlusion or underlying maculopathy were excluded from the study.
The authors concluded that baseline pseudodrusen in the fellow eye of CATT participants were associated with approximately 2 times higher risk of late AMD through 2 years. Pseudodrusen were associated independently with a higher incidence of nAMD (dot pseudodrusen) and GA (confluent pseudodrusen). These findings indicate that pseudodrusen should be considered alongside the AREDS severity score for the prediction of late AMD.
The average baseline subfoveal choroidal thickness in eyes with macular edema due to a RVO ranged from 210-364 microns and ranged from 165-311 in the fellow unaffected eye. While there was a significant reduction in the subfoveal choroidal thickness from baseline at months 1 and 3 in the affected eyes, following intravitreal Dexamethasone implant injection, there was no significant difference at month 1 and month 3 between the treated and unaffected eyes. However, at month 5 the subfoveal choroidal thickness was significantly higher in the affected eyes. At month 1 and 3 the subfoveal choroidal thickness was not significant among the BRVO and CRVO groups, but at month 5 the thickness had significantly increased as compared to month 3 in the CRVO group. There was no significant difference in choroidal thickness at months 1 and 3 among the ischemic and nonischemic occlusions, but at month 5 the ischemic eyes shows significant increase in thickness.
In conclusion, many studies have reported that various retinal and chorioretinal disorders can alter choroidal thickness. This retrospective study demonstrates that the subfoveal choroidal thickness is significantly higher in RVO eyes with macular edema and that intravitreal dexamethasone implants can decrease choroidal thickness. Since the choroidal vasculature plays an important role in retinal homeostasis, studying the choroidal structure may be an additional important aspect in determining a therapeutic response.
Esen, E, Sizmaz, S, et al. Retina. December 2016. 36(12): 2297-2303

|
ANSWER
TO "YOU MAKE THE DIAGNOSIS"
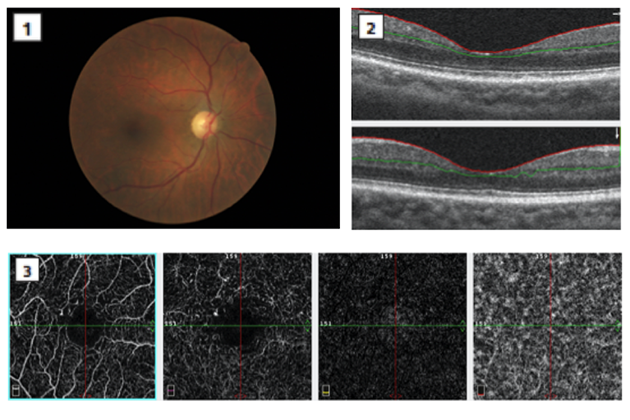
This shows an Optical coherence tomography angiography (OCTA) of a 79-year-old diabetic female. Fundus examination appeared normal with the exception of a small retinal hemorrhage and paramacular microaneurysms (Figure 1). SD-OCT b-scans showed microaneurysms in the inner retina consistent with the clinical picture (Figure 2). OCT Angiography of the superficial and deep capillary plexi visualize an enlarged foveal avascular zone (FAZ), capillary dropout, microaneurysms and vascular network alterations around the FAZ. (Figure 3)
Optical coherence tomography angiography (OCTA) uses a motion contrast imaging system in conjunction with volumetric angiographic data to provide a high-resolution 3-dimensional angiogram. The OCTA provides a segmentation map whereby the retinal vasculature is segregated into individual layers that correlate anatomically with the retina. The OCT angiograms can be analyzed from the anterior internal limiting membrane to the choroid to precisely identify the location of microvascular abnormality and can be cross-referenced with the B-scan images.
In diabetes, even in the absence of significant retinopathy, OCTA highlights changes in the macular capillary network that precede visible evidence of retinopathy on clinical examination. These changes include enlargement of the FAZ, increased visualization of the capillary network of the macula including alterations in caliber and morphology as well as evidence of nonperfusion. This technology is providing earlier identification of retinal insult ultimately optimizing patient care.
Julie Rodman, OD, FAAO
ORS fellow |

IN THE
NEWS
 |
Adherence to a Mediterranean diet may lower odds of neovascular AMD
A diet high in fish or omega-3 fatty acids can be protective against age-related macular degeneration, so those who adhered to a Mediterranean diet had lower odds of developing the disease, according to study in Ophthalmology.
Researchers included 5,060 randomly sampled people ages 65 years and older from seven study centers in Europe — United Kingdom, Estonia, Norway, France, Italy, Greece and Spain — in a cross-sectional, population-based epidemiologic study. All participants underwent an eye examination and digital retinal photography, and their dietary intake in the previous year was assessed using a semiquantitative food frequency questionnaire to determine their Mediterranean diet score.
Full dietary information was available for 4,753 participants; of those, 109 had neovascular AMD, 2,333 had early AMD, 2,262 did not have signs of AMD, and 49 had geographic atrophy. Six hundred forty-one participants had large drusen.
Higher Mediterranean diet scores were associated with lower odds of developing wet AMD. Compared with participants who had lower scores, those with high scores showed significantly lower odds of wet AMD (P = .01).
|
 |
PLEX Elite 9000 from Zeiss receives FDA clearance
The FDA has cleared the PLEX Elite 9000 for advanced retina research, Carl Zeiss Meditec announced in a press release.
This is the FDA’s first clearance for swept-source OCT imaging technology for posterior ocular structures, the release said.
The platform, which consists of swept-source OCT as well as OCT angiography, provides wide-field high-resolution imaging of the microstructures and microvasculature of the posterior segment.
U.S. members of the Advanced Retina Imaging (ARI) Network, a global consortium of clinicians and scientists who work in retinal disease research, may be able to enroll patients more easily and facilitate faster Institutional Review Board reviews for research approval because of the FDA clearance, according to the release.
“This instrument opens up a new world of structural and microvascular clarity. By imaging deeper and in greater detail than ever before, we will further our understanding of the retina and choroid, and greatly facilitate clinical trial investigations into different diseases,” Philip J. Rosenfeld, MD, PhD, chairman of ARI Network, said in the release.
There is a limited release of the PLEX Elite 9000 platform for retina research
|
 |
UC Irvine Health to receive $5 million gift for retinal research from Gavin and Ninetta Herbert
Gavin Herbert, the founder of Allergan, and his wife, Ninetta, will give $5 million to UC Irvine Health’s Gavin Herbert Eye Institute to advance retinal research, the university announced in a press release.
Between 25 and 30 investigations are ongoing at the institute at any time, the release said, ranging from engineering an artificial cornea to treatment for blepharospasms. This gift will be dedicated to expanding research into the retina.
“Many people worked long years to complement industry with a world-class academic eye center that would be an innovative partner and also provide the highest quality of care for the community,” Gavin Herbert said in the release. “With that now in place at the Gavin Herbert Eye Institute, our gift will sustain the research that is vital to the institute’s long-term reputation as a global leader.”
|
 |
Study to evaluate elamipretide for dry AMD
The ReCLAIM phase 1 study evaluating the use of elamipretide for intermediate age-related macular degeneration has been initiated, according to a press release from Stealth BioTherapeutics.
The open-label study will evaluate elamipretide’s safety and tolerability through 12 weeks of treatment with daily subcutaneous injections, the release said. Patients will be age 55 years or older and have at least one eye with intermediate AMD, as well as either drusen on the retina without geographic atrophy or geographic atrophy with an unaffected central fovea.
“There are currently no FDA-approved treatment options for dry AMD, so we are eager to better understand the effect that elamipretide may have in treating these roughly 13 million patients,” Scott Cousins, MD, the trial investigator, said in the release.
Top-line data are expected in mid-2017.
|
 |
Santen releases topline results supporting efficacy, safety of Opsiria for non-infectious uveitis
Topline results for the SAKURA phase 3 program show the efficacy and safety of Opsiria as a potential treatment for non-infectious uveitis of the posterior segment, Santen announced in a press release.
Opsiria (440 μg sirolimus injection), an intravitreal, locally delivered, targeted immunoregulator, was shown to reduce intraocular inflammation effectively and safely, as measured by vitreous haze, the release said.
Santen now plans to file a new drug application to the FDA based on the data from the program.
|
 |
Combination of squalamine, ranibizumab improves BCVA in eyes with retinal vein occlusion
Patients with macular edema secondary to retinal vein occlusion who received a combination of squalamine and ranibizumab had a better improvement in best corrected visual acuity than patients who received ranibizumab alone, according to a study in Ophthalmic Surgery, Lasers and Imaging Retina.
The single-center, open-label, randomized trial included 20 eyes of 20 consecutive patients; nine eyes had nonischemic central retinal vein occlusion, eight eyes had branch retinal vein occlusion, and three eyes had hemicentral retinal vein occlusion.
Study eyes received a combination of topical squalamine (OHR-102, Ohr Pharmaceuticals) and intravitreal Lucentis 0.5 mg (ranibizumab, Genentech) for 10 weeks and then were randomized to continue or discontinue squalamine. Thirteen treatment-naïve control eyes from previous studies received ranibizumab 0.5 mg at baseline and then monthly for 6 or 7 months.
At baseline, the mean best corrected visual acuity was 55.6 ETDRS letters in the squalamine group and 55 ETDRS letters in the control group. Patients in the combination group had a mean improvement of 25.6 letters at 38 weeks, compared with a mean improvement of 16.3 letters in the control group at 9 months.
|
 |
Sun Pharma launches BromSite in US
BromSite for the treatment of postoperative inflammation and prevention of ocular pain is now available in the United States, Sun Pharma announced in a press release.
BromSite (bromfenac ophthalmic solution 0.075%) was approved by the FDA on April 8 and is the first NSAID approved to prevent ocular pain and treat eye inflammation after cataract surgery, the release said. It is also the first branded product launched by Sun Pharma in the United States.
“Clinical studies have reinforced BromSite’s strong safety and efficacy profile in cataract surgery patients, culminating in this FDA indication for the prevention of ocular pain following surgery,” Abhay Gandhi, CEO, North America Business, Sun Pharma, said in the release. “We are confident BromSite will prove itself a quality treatment option for cataract surgeons and their patients.”
|
 |
Revenues, net income increase in third quarter for Regeneron
Regeneron reported total revenues of $1.2 billion in the third quarter compared with $1.1 billion in the third quarter of 2015, an increase of 7%, according to a press release.
This included $857 million in net product sales from Eylea (aflibercept), an increase from $738 million in the third quarter of last year.
GAAP net income was reported at $265 million, or $2.53 per basic share and $2.27 per diluted share, compared with $210 million, or $2.04 per basic share and $1.82 per diluted share, a year ago.
Research and development costs rose from $426 million a year ago to $543 million in the third quarter, which was attributed to a $25 million upfront payment for a license and collaboration agreement with Adicet and higher development costs.
|
 |
Ophthotech reports $60.9 million loss in third quarter
Ophthotech reported a net loss of $60.9 million, or $1.71 per diluted share, in the third quarter of 2016, whereas a net loss of $39.6 million, or $1.14 per diluted share, was reported in the third quarter of 2015.
The company spent $10.4 million more on research and development in the third quarter of 2016 than in the same quarter of 2015, that is, $50.9 million compared with $40.5 million. The increase was attributed mostly to the Fovista (pegpleranib) phase 3 clinical trials program, according to a company press release.
Collaboration revenue was reported at $1.7 million for the quarter, down from $3.4 million in the third quarter of 2015.
|

MEET
THE FELLOWS
In each issue, a Fellow of the Optometric Retinal Society is highlighted. In this issue, Dr. Anthony Van Alstine, a new ORS fellow, will be highlighted
Dr. Anthony Van Alstine practices full scope optometry and serves as clinical externship supervisor at the WJB Dorn VA Medical Center in Columbia, SC. He graduated from the Indiana University School of Optometry as the valedictorian of the OD Class of 2011 and completed an optometric residency after graduation. He achieved a Master’s Degree in vision science at Indiana University in 2012 with his research focusing on the quantification of retinal ganglion cell function using the multifocal electroretinogram. His research has been presented at AAO, ARVO, ISCEV, and ISER meetings. Dr. Van Alstine has a passion for clinical education and holds adjunct faculty status at six ACOE accredited schools of optometry. He teaches optometry externs and residents in clinic on a daily basis. He also enjoys lecturing on a wide variety of optometry topics and frequently provides COPE approved continuing education to his colleagues. He is a fellow in the American Academy of Optometry and currently serves as the president of the South Carolina Chapter of the American Academy of Optometry. His greatest joys in life are his wife and three sons. He enjoys spending time with his family, many different outdoor activities, and serving in his local church.
SPONSOR NEWS

Editor
in Chief
Steven Ferrucci, OD, FAAO
Co-Editor
Mark T. Dunbar, OD, FAAO |
Journal
Reviewers
Celina Diego, OD
Tea Avdic, OD
Steve Quan, OD
Angela Diamantakos, OD
Faten Edriskhalaf, OD
Jenna Blechman, OD
Senior Graphic Designer
Matt Egger
|
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|