| |
Volume 13, Number 2 |
June 2017 |
|
|
Inside
This Issue |
|
|
|
|
|
This e-newsletter is provided free to doctors through industry support from |
 |
| |
FROM
THE DESK OF THE EDITOR
Every other week I sit down with a few clinic colleagues, our resident, and our fourth-year students for journal club. We spend a few of these meetings dedicated to AMD. At some point, we go over nutrition and genetic testing. It is always interesting for me to hear what the students have learned at other rotation sites and whether or not other practitioners are recommending genetic testing. Every time when this discussion comes up, I am not able to give the students a firm answer to the following questions: How much zinc is the right amount, and who needs it? I, personally, seek genetic testing before recommending vitamin supplements (specifically 25mg or 80mg zinc) to a patient with intermediate AMD. This is due to a fear of potentially causing harm to a patient with high complement factor H (CFH) risk alleles.
Dr. Carl Awh first brought to our attention a concern with high doses of zinc in patients with a particular genetic profile (high CFH) in 2013. As you can read in the abstract section below, Dr. Awh has added another twist to the plot, this time regarding antioxidant supplementation. Depending on a patient’s genetic profile, are some patients harmed with an increased risk of developing AMD by taking high-dose antioxidants while others are protected? So once again, we have more uncertainty in what supplements to use and how much to tell our patients to take. How do you address nutrition in AMD? I’d love to hear your thoughts.
Anna Bedwell, OD, FAAO
Editor-in-Chief |
 |
PRESIDENT'S MESSAGE
Summer is upon us! That means warm weather, barbeques and bikinis! Unless you live in Southern CA like me, where that’s what we do year round. So I hope everyone has fun, goes on vacation and doesn’t get too sunburned. And remember to wear sunglasses, as UV is bad for AMD!! Also, I find summer a good time to catch up on some reading, whether it is about your favorite retinal disease (mine’s AMD) or a trashy summer novel (I would recommend “Big Little Lies” by Liane Moriarty. Better than the HBO mini-series).
Also, I would like to share some exciting news. We, at the ORS, decided to start a Larry Alexander Resident Case Report Contest for current residents to honor our old friend, former ORS president and a true retinal pioneer, Larry Alexander, who passed away in April 2016. We had 12 applicants in the contest, which was not bad for the first year. Dr. Julie Rodman and Dr. Bill Denton and the rest of their amazing committee reviewed the cases and had a difficult time choosing a winner from a variety of interesting and excellent cases. The winner of the first Larry Alexander Resident Case Report is Kathryn Dailey, OD, from VA Puget Sound. Her topic was acute syphilitic posterior placoid chorioretinitis in a heterosexual female. She will get $2,500, sponsored by Optovue and Macuhealth, and her article will also be published in the June edition of Review of Optometry. We are looking forward to carrying this tradition into the future, and hopefully will get even more applications down the road.
Lastly, I am pleased to announce we will be having our annual ORS Meeting, Retina Update 2017, this December 1-2, at the Sheraton Park Hotel in Anaheim Calif. We will be offering a minimum of 14 hours of exciting and innovative education by ORS members as well as a world-renown retinal specialist. Stay tuned for more information in coming months. I hope to see you there!
Sincerely,
Steven Ferrucci, OD, FAAO
ORS President

YOU
MAKE THE DIAGNOSIS
Answer appears later in newsletter.

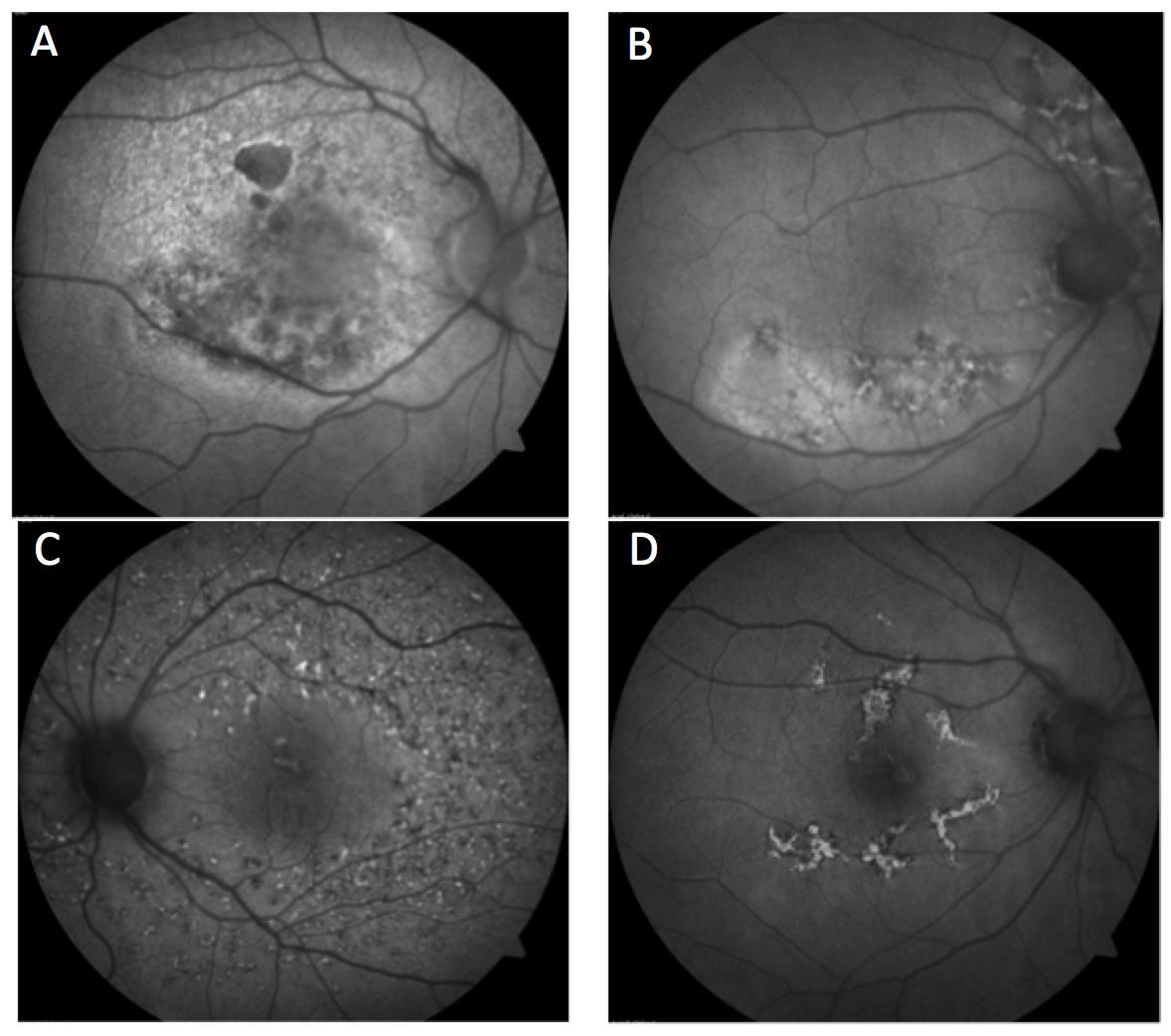
IMAGE GALLERY
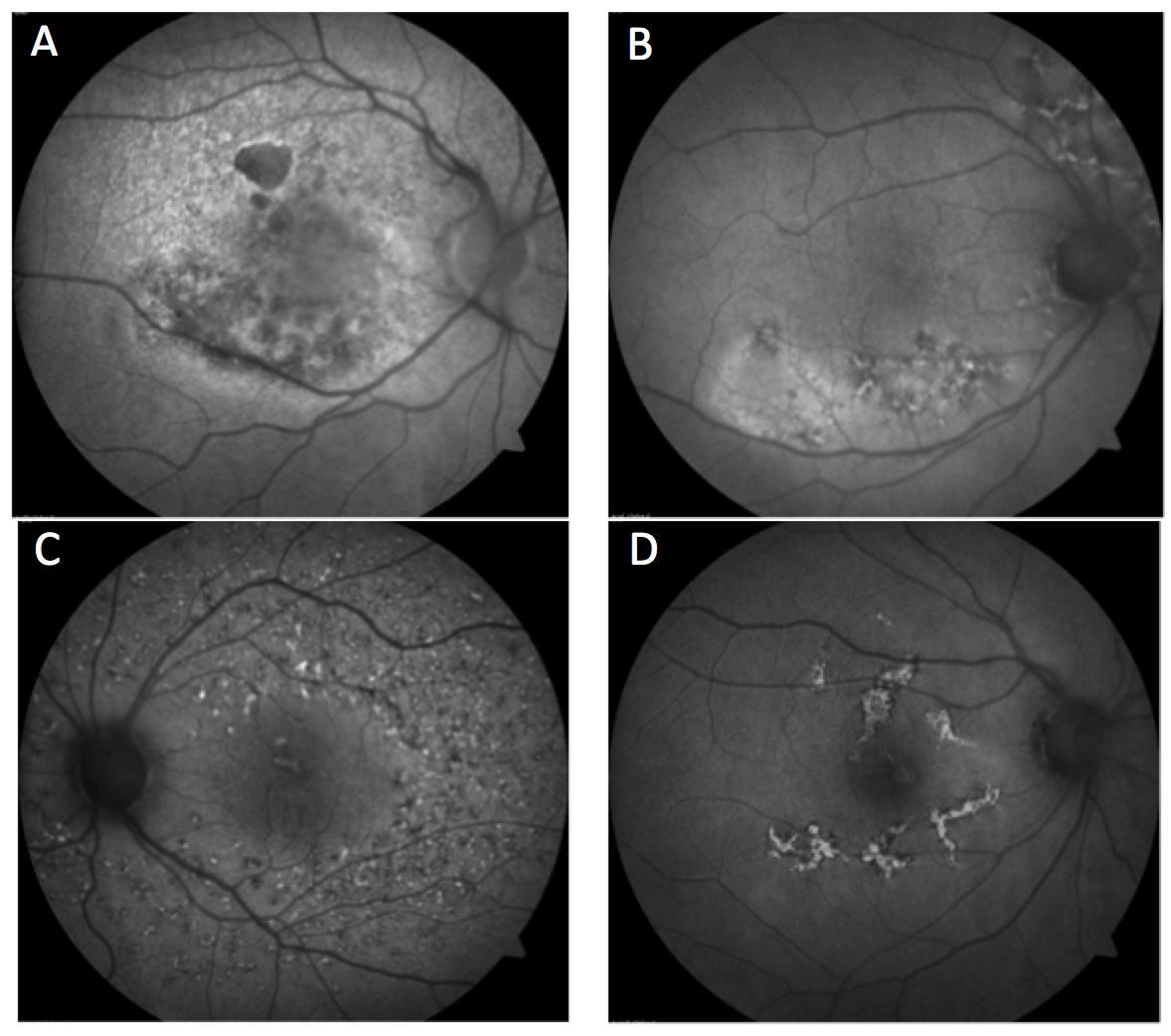
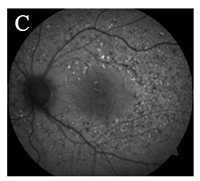
Which of the following fundus autofluorescence images represents fundus flavimaculatus?
Answer appears later in newsletter.
|

JOURNAL
ABSTRACTS
Adherence to Hydroxychloroquine Dosing Guidelines by Rheumatologists
This was a retrospective review of electronic medical records to determine the impact of hydroxychloroquine dosing guidelines set by the American Academy of Ophthalmology in 2011 and 2016. All patients were seen in both rheumatology and ophthalmology within an integrated health care system. Patient’s weight, height, gender and HCQ dosage were all available through EMR. Maximum HCQ doses were calculated using both the 2011 and 2016 guidelines. The 2011 guidelines recommended a maximum of 6.5mg/kg based on ideal body weight. The 2016 guidelines recommended a maximum of 5mg/kg of actual body weight. The study had 554 patients who were started on HCQ after 2009, 92 of whom started on HCQ before the 2011 guidelines were published. The authors found that over half (54%) of those patients were started on an excess dose based on the 2011 guidelines. Furthermore, after the 2011 guidelines were published, dose reductions were rare at only 7%.
The authors also analyzed 527 patients currently on HCQ by the 2016 guidelines and found a similar trend with just over half receiving an excess dose. In particular, 43% (224/527) were prescribed doses more than 50 mg above the actual body weight calculated target.
This paper demonstrates that the AAO’s published guidelines have had little impact on prescribing of HCQ by rheumatologists. The current formulation of the drug negatively impacts flexibility in prescribing as it only comes in a 200mg tablet. The authors suggest utilization of prescribing prompts within EMR systems to promote guideline adherence.
Braslow RA, Shiloach M, Macsai MS. Adherence to hydroxychloroquine dosing guidelines by rheumatologists: an electronic medical record-based study in an integrated health care system. Ophthalmology. 2017 May;124(5):604-8.
Differential Macular Features on Optical Coherence Tomography Angiography in Eyes with Choroidal Nevus and Melanoma
This retrospective analysis compared optical coherence tomography angiography (OCTA) features of eyes with choroidal nevus and melanoma to their unaffected eye. There were 70 patients with choroidal nevus and 36 patients with choroidal melanoma, all macular or extramacular in location. Contralateral eyes had no existing macular pathology.
OCTA measurements included central macular thickness (CMT), foveal avascular zone (FAZ) and capillary vascular density (CVD). Patients with choroidal nevus had a similar CMT, FAZ and CVD compared with their normal, unaffected eye.
Most notably, CMT was considerably thicker in eyes with melanoma (322µm vs. 259µm). This did not correlate with tumor thickness. In the melanoma group, the deep FAZ area was larger than in the superficial FAZ in both the normal and affected eyes. The authors also reported that the deep FAZ was much larger in specifically submacular melanoma eyes over their normal counterparts, while the superficial FAZ measurements were similar between each eye. The deep CVD was decreased in melanoma eyes in contrast to the unaffected eyes regardless of presence of subretinal fluid.
The authors proposed that these OCTA features could be helpful in differentiating between choroidal nevus and melanoma.
Valverde-Megías A, Say EA, Ferenczy SR, et al. Differential macular features on optical coherence tomography angiography in eyes with choroidal nevus and melanoma. Retina. 2017 Apr;37(4):731-40.
Diabetes Alters the Magnitude of Vitreomacular Adhesion
Vitreomacular adhesion is a commonly encountered finding on OCT in which there is partial detachment of the vitreous in the perifoveal area without the presence of traction. This study investigated the presence and amount of vitreomacular adhesion specifically in diabetic eyes. They analyzed 141 diabetic patients and 250 age- and gender-matched normals. Diabetic patients with PDR or DME were excluded. The patients ranged from 20 to 80 years old. Patients all had a 25 line raster SD-OCT (Spectralis) scan of the macula and a complete exam to determine the clinical presence of PVD. In cases of partial PVD with VMA, the Spectralis software was able to quantify the area of attachment in mm2.
The authors found a significant difference in the VMA area between the diabetic and normal groups. The diabetic group retained VMA longer over the control group, particularly in comparing the later decades of life. At mean age 56 years in the normal group, there was 50% release of the posterior hyaloid area from the macula. In contrast, in the diabetic group this occurred at a mean age of 72 years. The diabetic group achieved complete PVD at an older age compared to controls.
The results suggest that diabetes caused a stronger and prolonged attachment between the vitreous and retina. Other studies have shown that PVD offers a protective effect from developing DME. Thus, the authors proposed that quantifying the amount of VMA in diabetics might be useful in the management of DME.
Nesmith BL, Palacio AC, Schaal Y, et al. Diabetes alters the magnitude of vitreomacular adhesion. Retina. 2017 Apr;37(4):749-52.
Predictive Value of Optical Coherence Tomographic Features in the Bevacizumab and Ranibizumab in Patients with Diabetic Macular Edema (BRDME) Study
Noninvasive imaging provided by optical coherence tomography (OCT) delivers the invaluable ability to assess retinal integrity, pathological retinal changes and fluid accumulation. In evaluation of specific OCT parameters as potential biomarkers in patients receiving anti-vascular endothelial growth factor (VEGF) therapy for diabetic macular edema (DME), serous retinal detachment (SRD) and disorganization of retinal inner layers (DRIL) were identified as predictive factors of visual acuity improvement.
Expanding on the framework of the BRDME study, the researchers evaluated a group of OCT parameters as potential biomarks. These biomarkers included serous retinal detachment (SRD), vitreomacular adhension (VMA), external limiting membrane (ELM), inner/outer segment junction (IS/OS line) and disorganization of retinal inner layers (DRIL), most of which were previously examined via retrospective and single medical center studies. By utilizing the parameters of a large, multicenter cohort study, authors were able to provide a more definitive predictive value of treatment responses of patients with DME to anti-VEGF therapy.
THE BRDME study is an ongoing multicenter, longitudinal study that compares the results of DME treatment via bevacizumab and ranibizumab. Study participants were at least 18 years of age, had Type 1 or Type 2 diabetes with HbA1c less than 12%, had been diagnosed with clinically significant DME as defined by the Early Treatment Diabetic Retinopathy Study and a best-corrected visual acuity (BCVA) between 20/25 to 20/400. Patients with proliferative diabetic retinopathy, previous ocular surgeries or significant ocular disease, apart from diabetic retinopathy, were excluded from the study.
The results emphasized two statistically significant biomarkers. The presence of serous retinal detachment at baseline was associated with significant improvement in BCVA at three- and six-month follow-up. Meanwhile, the presence of disorganization of retinal inner layers was associated with lower BCVA at three- and six-month follow-up.
Approximately half of patients with DME fail to obtain complete resolution on anti-VEGF treatment. These findings support the ability to use baseline retinal appearance to predict good and poor treatment responders prior to initiating treatment.
Fickweiler W, Schauwvlieghe AM, Schlingemann RO, et al. Predictive value of optical coherence tomographic features in the bevacizumab and ranibizumab in patients with diabetic macular edema (brdme) study. Retina; Apr 2017. [Epub ahead of print].
Factors Associated with Worsening Proliferative Diabetic Retinopathy in Eyes Treated with Panretinal Photocoagulation or Ranibizumab
The intention of the study was to compare rates of events that represent worsening of proliferative diabetic retinopathy (PDR) in eyes treated with panretinal photocoagulation (PRP) or ranibizumab. In addition, the study examined what, if any, anatomical predictive factors to said events existed.
Using the published data of two-year primary outcome results comparing panretinal photocoagulation with intravitreal ranibizumab in a randomized clinical trial of 394 eyes with PDR without history of previous treatment, authors measured time to the first occurrence of vitreous hemorrhage, retinal detachment, anterior segment neovascularization or neovascular glaucoma. These events represented progression in PDR despite treatment.
Following two years of observation, the probability of worsening PDR in patients managed via PRP was 42% vs. patient managed with intravitreal ranibizumab, which was 34%. In addition, pattern scan PRP treatments were less effective in reducing progression (60%) than conventional single-spot PRP (39%). More severe baseline levels of diabetic retinopathy were predictive of increased likelihood of worsening PDR. Eyes with visually significant diabetic macular edema at baseline were isolated in subgroup, as they were required to have intravitreal ranibizumab injections. In these eyes, progression in PDR was still less likely than in patients treated with PRP.
This study further supports the benefits of anti-vascular endothelial growth factor treatment as an alternative PRP intervention over a two-year period. That stated, authors wrote that PRP still represents significant benefits in that it requires less frequent visits and may be more cost effective for many patients.
Bressler SB, Beaulieu WT, Glassman AR, et al. Factors associated with worsening proliferative diabetic retinopathy in eyes treated with panretinal photocoagulation or ranibizumab. Ophthalmology 2017 Apr;124(4):431-9.
Progression From No AMD to Intermediate AMD as Influenced by Antioxidant Treatment and Genetic Risk: An Analysis of Data From the Age-Related Eye Disease Study Cataract Trial
The use of genetic testing in the management of age-related macular degeneration (AMD) is certainly controversial. Different groups have studied data from the original Age-Related Eye Disease Study (AREDS) and have reached varying conclusions. Most of the controversy revolves around the role of high-dose zinc in the management of AMD, and whether or not it has the potential to actually be harmful to some individuals with certain genetic profiles. The response to zinc may be related to the presence and number of two particularly important risk alleles, CFH and ARMS2. An individual can carry either 0, 1, or 2 of each of these alleles.
The AREDS study was designed to examine the rate at which patients with some level of non-advanced AMD progressed to advanced AMD over time. Patients who were enrolled in the study but did not have AMD were placed in a study arm that evaluated the effect of antioxidant supplements (namely 15mg of beta carotene, 500mg of vitamin C and 400 IU of vitamin E but no zinc) vs. placebo on the progression of cataracts. The current article uses this AREDS study group to examine the effect of antioxidants on the risk of progressing from no AMD to intermediate AMD over approximately eight years.
Caucasian patients with available DNA were included in the analysis, and were stratified based upon the total number of CFH and ARMS2 risk alleles that they carried. The number of patients meeting the study criteria was 554, and after four were excluded for progressing straight to advanced disease, 550 were ultimately analyzed. The results were fascinating.
The risk of developing intermediate AMD over the study period was very highly linked to the total number of genetic risk alleles that were present. Individuals with zero risk alleles had only a 6.5% chance of going from no AMD to developing intermediate AMD, while those with 3 or 4 risk alleles had a 39% chance. Overall, there was no statistically significant difference in the progression rate of individuals taking antioxidants and those taking a placebo. However, a closer examination of the multiple genetic subgroups revealed a much different story. Patients in the low genetic risk category, those with 0 or 1 risk allele, had a substantially greater chance of developing intermediate AMD when taking antioxidants, with a hazard ratio of 2.31. Those in the high genetic risk category carrying 3 or 4 risk alleles had a significantly lower chance of developing intermediate AMD when taking antioxidants, with a hazard ratio of .27. For patients with average genetic risk carrying 2 alleles, antioxidants had no significant effect.
So it appears, at least based upon this analysis, that antioxidant supplements might have a protective effect for some people without AMD while potentially having a harmful effect for others. Much like the debate over zinc supplementation in the treatment of AMD, this analysis calls in to question the paradigm of having a one-size-fits-all supplement recommendation for all individuals. Instead, personalized recommendations based upon an individual patient’s genetic profile may, in time, prove to be a more effective model in reducing the disease burden of AMD.
Awh C, Zanke B, Kustra R. Progression from no amd to intermediate amd as influenced by antioxidant treatment and genetic risk. Journal of Vitreoretinal Diseases 2017;1(1):45-51.
Poppers: Legal Highs With Questionable Contents? A Case Series of Poppers Maculopathy
This case report series from England examines 12 patients who suffered from poppers maculopathy. Poppers are liquids composed of isopropyl alcohol and isopropyl nitrate, often in a roughly equal mixture. They are marketed under many different names, and are abused for their psychoactive effects and properties of sexual arousal, most notably in the homosexual male population. Products include Platinum, Liquid Gold, Rush, Jungle Juice and many others (often with X-rated names).
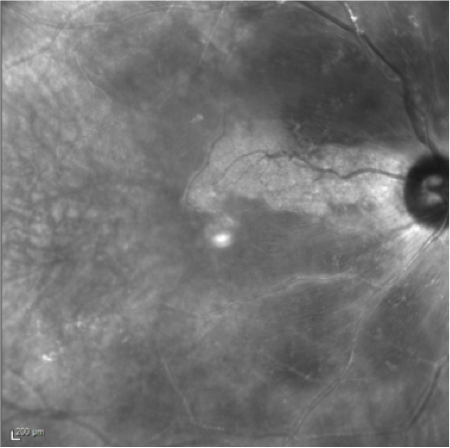
It is believed to be the isopropyl nitrate that leads to maculopathy via a mechanism that is poorly understood. Theories include prolonged nitrous oxide production with subsequent photoreceptor toxicity and possible interference with zeaxanthin’s protective effects, thus leading to light toxicity. Patients suffering from poppers maculopathy complain of a disturbance or scotoma in the central vision. This is typically noted in both eyes, but may occur in just one. Upon funduscopic examination, a small, yellow lesion is seen in the fovea. FAF imaging reveals hyperfluorescence of the lesion, while SD-OCT scans exhibit disruption of the inner and outer photoreceptor segment junction in the area of the photoreceptor integrity line (PIL). The OCT images look very similar to those seen with solar maculopathy and laser maculopathy, thus leading to speculation regarding a mechanism similar to light toxicity.
There is no effective treatment for popper maculopathy, so the only course of action is to discontinue use of poppers. Most patients make at least a partial recovery from both a symptom and a structural standpoint, with many actually experiencing a complete recovery.
Rewbury R, Hughes E, Purbrick R, et al. Poppers: legal highs with questionable contents? A case series of poppers maculopathy. Br J Ophthalmol; Apr 2017. [Epub ahead of print].
Intravitreal Anti-VEGF Injections Reduce Aqueous Outflow Facility in Patients With Neovascular Age-Related Macular Degeneration
It is well-known that intravitreal steroid injections can lead to a significant elevation of intraocular pressure (IOP). It is less commonly known that Anti-VEGF injections with Lucentis, Avastin or Eyelea also have a small chance of causing elevated IOP. The mechanism is unknown, but it is believed to be related to a decrease in aqueous outflow through the trabecular meshwork.
This study was conducted to examine risk factors that may be associated with an increased chance of IOP elevation. Patients receiving anti-VEGF shots in just one eye for neovascular AMD with any of the three common agents listed above were included. A total of 42 such patients were studied and were broken down into categories. One category was patients who had received less than or equal to 10 injections, while a second category consisted of patients who had received 20 or more injections. There were 20 eyes in the low injection category, and 22 in the high injection group. Patients were further divided in to those with ocular hypertension in the non-injected eye, which was defined as a pressure over 21mmHg, and those without ocular hypertension in the non-injected eye. Patients being treated for glaucoma were excluded. In all groups, the trabecular meshwork outflow facility was measured using tonography. In patients with less than or equal to 10 injections, no decrease in outflow facility was observed. In patients in the high injection group (greater than or equal to 20 injections), however, the trabecular meshwork outflow facility was found to be 12% lower on average than in the patient’s fellow eye. Additionally, there were five patients with both a high number of injections and ocular hypertension in the fellow eye. In these five individuals, the average decrease in outflow facility was 46% on average.
So it appeared that there are at least two risk factors for elevated IOP after receiving anti-VEGF injections. Such elevations appeared to occur after larger numbers of repeated injections, and they appeared to be more common in patients with pre-existing ocular hypertension, likely due to the trabecular outflow in such eyes already being compromised. Researchers wrote that it is important for practitioners to be aware of these risk factors in patients receiving multiple anti-VEGF injections and to monitor such patients closely for clinically significant elevations in IOP.
Wen JC, Reina-Torres E, Sherwood JM, et al. Intravitreal Anti-VEGF injections reduce aqueous outflow facility in patients with neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 2017;58:1893-8.

 |
 |
|
ANSWER
TO "YOU MAKE THE DIAGNOSIS"
Retinal Morphological Changes Noted on Optical Coherence Tomography in Cilioretinal Artery Spared Central Retinal Artery Occlusion
Introduction:
The Optical Coherence Tomography (OCT) findings in acute and chronic phases of central and branch retinal artery occlusion are well-established in the literature. The following is a case of a cilioretinal artery-spared central retinal artery occlusion, showing the comparison of the affected retina as compared to the arterial spared normal remaining retina in both acute and late phase of the disease.
Case Report:
A 70 year-old white female presents for evaluation of sudden onset vision loss of the right eye. Patient is a past smoker and has been under medical care for systemic hypertension and arthritis with nonspecific joint and general pain. Her current medications are: Aleve once daily, glucosamine-chondroitin, multivitamin, vitamin D3 400 units, calcium, aspirin 81mg/day, cyclobenzaprine 10mg/day, escitalopram 10mg/day, ranitidine 150 mg/day and valsartan-hydrochlorothiazide.
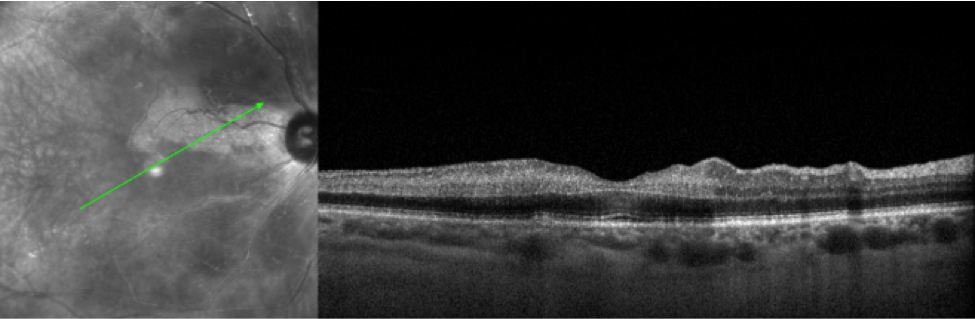
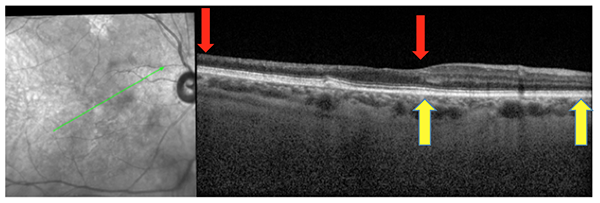
Examination was remarkable for VA OD: CF@4’ and OS: 20/30. IOP was 9 OD/OS. Pupillary testing was not done as the patient presented with dilated pupils from the referring optometrist office. Confrontation field was restricted in the right eye and normal in the left eye. Slit-lamp examination was remarkable for 1+ nuclear sclerosis cataracts in each eye. Fundus exam of the right eye revealed significant retinal whitening with a cherry red macula in an arcuate pattern with normal color retina within the distribution of the cilioretinal artery in the right eye and unremarkable findings in the in the left eye. The OCT showed increased reflectivity (hyperreflectance) and thickening of the inner retina in the ischemic region with the perfused spared area remaining normal (Image 1).
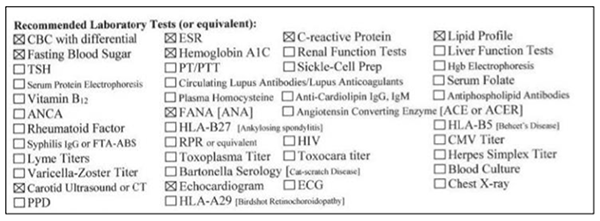
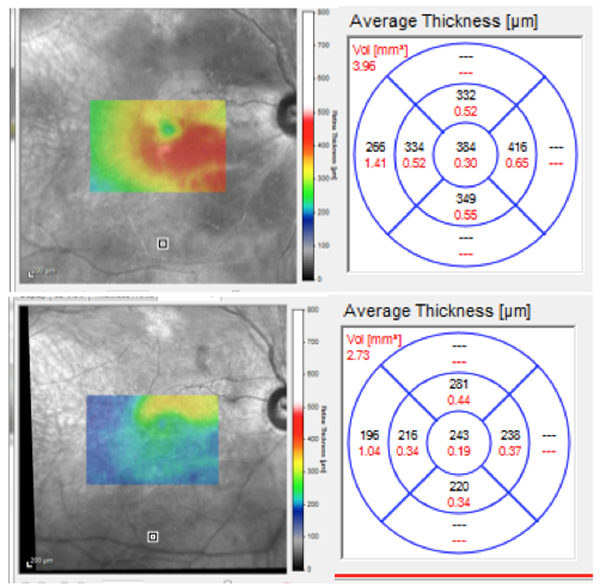
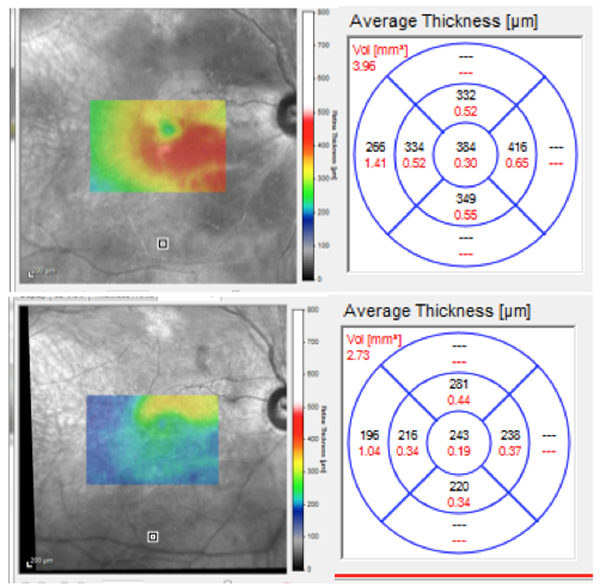
Patient was diagnosed with a cilioretinal artery-spared central retinal artery occlusion (CRAO) and was instructed to increase aspirin to 321mg daily and was referred for medical workup listed in Figure 1. Patient’s medical workup subsequently led to diagnosis of giant cell arteritis and polymyalgia rheumatic, currently under management by rheumatology. Two months later, VA had recovered to 20/100 and the area of retinal whitening had normalized on fundus examination. The OCT finding was remarkable for atrophy of the inner retina in the affected area where the spared area remained normal (Image 2) the central retinal thickness (CRT) had decreased by 140um (Image 3) due to ischemic atrophy of the inner retina. At six-month follow-up, patient’s examination and OCT findings were unchanged. Her systemic disorders were well-controlled with improved symptoms of general pain.
Discussion:
Optical coherence tomography (OCT) can play an important role in diagnosis and management of a wide variety of posterior segment disorders. The OCT characteristics of branch (BRAO) and central retinal artery occlusion (CRAO) in both acute and late phase of these conditions have been well-described in the literature. 1-5
These findings are described as hyper-reflectivity and increased thickness of the inner retina in the affected hypoxic areas with decreased reflectivity of the outer retina due to optical shadowing of the thickened overlying retina.1-5 These findings are consistent with what is observed in the case presented here. The late OCT characteristics for BRAO and CRAO are consistent with atrophy and thinning of the inner retina as a result of ischemic atrophy.1-5 This also can be seen in the follow-up of this case.
Conclusions:
OCT findings are reliable and repeatable in BRAO and CRAO and the technology can assists eye-care practitioners in diagnosis of these and many other posterior segment conditions.
Mohammad Rafieetary, OD, FAAO
ORS Fellow
|
Figure 1
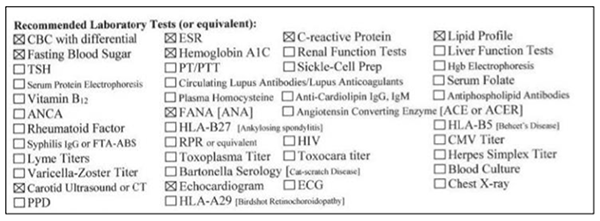
Image 2: Two month follow-up of the patient shows thinning of the inner retina (between red arrows) with spared areas remaining normal (between yellow arrows).
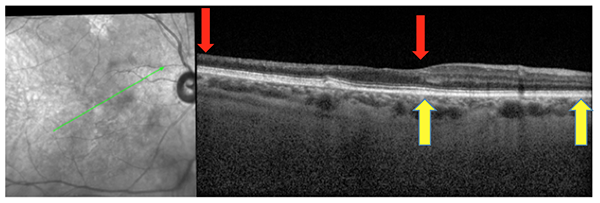
Image 3: Initial thickness map shows central retinal thickness at 384 (top) decreased to 243 (bottom) at two months follow-up.
References:
1) Falkenberry SM, Ip MS, Blodi BA, Gunther JB. Optical coherence tomography findings in central retinal artery occlusion. Ophthalmic Surg Lasers Imaging. 2006 Nov-Dec;37(6):502-5
2) Schmidt D, Kube T, Feltgen N. Central retinal artery occlusion: findings in optical coherence tomography and functional correlations. Eur J Med Res. 2006 Jun 30;11(6):250-2
3) Salinas-Alaman A, Garcia-Layana A, Heras-Mulero H, et al. Optical coherence tomography in central retinal artery occlusion. Arch Soc Esp Oftalmol. 2006;81:553-6
4) Shah VA, Wallace B, Sabates NR. spectral domain optical coherence tomography findings of acute branch retinal artery occlusion from calcific embolus. Indian J Ophthalmol. 2010 Nov-Dec; 58(6): 523-4
5) Karacorlu M, Ozdemir H, Arf Karacorlu S.Optical coherence tomography findings in branch retinal artery occlusion. Eur J Ophthalmol. 2006 Mar-Apr;16(2):352-3
|

IN THE
NEWS
 |
EyeGate Pharmaceuticals Partners with Valeant in Study of Iontopheresis
EyeGate has teamed up with Valeant’s Bausch + Lomb to study EyeGate’s own corticosteroid, EGP-437, in the treatment of post-cataract surgery inflammation and noninfectious uveitis via iontopheresis.
Iontopheresis is a “needle-less” method to deliver a specific amount of drug through the sclera by means of a low-level electrical current. The potential benefits of ocular iontophoresis over topical drops include higher targeted drug concentrations, greater bioavailability, longer therapeutic effect and less frequent dosing.
From their Phase Ib/IIa clinical trial for the indication of post-cataract surgery, EyeGate has already reported positive data for the drug/delivery system. A Phase III trial for the uveitis indication is under recruitment.
|
 |
Surgical Robot Performs Successful Injection in Patient with Retinal Vein Occlusion
University Hospitals Leuven in Belgium reported the first successful injection into a retinal vein using their own designed surgical robot. The robot utilizes a needle of just 30µm to inject ocriplasmin to break up the clot in the retinal vein. A Phase I trial has shown that this is technically feasible. Now a Phase II trial must demonstrate what the clinical effect is for patients suffering from RVO.
|
 |
NightstaRx Launches First Phase I/II Gene Therapy Clinical Trial for Retinitis Pigmentosa
NightstaRx is a biopharmaceutical company based in the UK and focused on gene therapy treatment for retinal dystrophies. It has recently begun enrollment for a multicenter, open-label trial of gene therapy for patients with X-linked retinitis pigmentosa (XLRP). According to NightstaRx, this is the first clinical gene therapy trial for XLRP. The treatment consists of a single subretinal injection of AAV-XLRPGR gene therapy. XLRP is inherited by males in a recessive pattern. It is caused by a mutation in the retinitis pigmentosa GTPase regulator (RPGR) gene. This treatment will use an adeno-associated viral vector to deliver a codon-optimized copy of the RPGR gene into the retina.
|
 |
Scientists Present Evidence of Ocular Effects From Prenatal Exposure to Marijuna
Scientists in São Paulo, Brazil, demonstrated that in utero exposure to marijuana leads to developmental effects in the eye. This research is the first to show effects from in utero cannabis exposure on the retina. The researchers subjected pregnant mice to marijuana smoke or filtered air throughout the pregnancy. The newborn mice were then studied at three, six and 12 months age. Those mice exposed to marijuana consistently had much thinner retinas than the controls. This research was presented at the 2017 Annual Meeting of the Association for Research in Vision and Ophthalmology (ARVO) in Baltimore. The abstract title is “Lasting Effects of Prenatal Marijuana Exposure on the Retina: An Experimental Study in Mice.”
|
 |
Lucentis Gains Further FDA Approval for Diabetic Retinopathy
Genentech revealed that the FDA has approved Lucentis (ranibizumab) 0.3mg for treatment of all forms of diabetic retinopathy. Previously, Lucentis only had the approval for diabetic retinopathy (DR) in patients with diabetic macular edema (DME). Now, Lucentis is the only FDA-approved medicine to treat DR with or without DME. Lucentis was given Priority Review by the FDA based on the results of the Diabetic Retinopathy Clinical Research Network’s (DRCR.net) Protocol S study. This study compared the anti-VEGF injection to panretinal laser treatment in DR with and without DME. Those in the Lucentis group improved and showed a decrease in level of retinopathy.
|
 |
Antibiotic Prophylaxis for Anti-VEGF Injections Associated with Higher Risk of Endophthalmitis
Data presented at the 2017 Annual Meeting of the Association for Research in Vision and Ophthalmology (ARVO) showed that patients who had antibiotic coverage prior to anti-VEGF injection had a 1.7 times higher risk of acquiring endophthalmitis over those who did not. The researchers from University of Santiago de Campostela in Santiago, Spain, analyzed a total of 276,774 injections. In the patients studied, about 40% had antibiotic prophylaxis and 60% did not. Location of the procedure site did not carry any effect (operating rooms vs. outpatient clinic). The authors concluded that antibiotic prophylaxis for anti-VEGF injections is unnecessary and may even carry a higher risk of harm. The abstract title is “The Effect of Antibiotic Prophylaxis on Endophthalmitis Rate After Intravitreal Injection With Antiangiogenic Agents: A Meta-Analysis.”
|

IMAGE QUIZ ANSWER
Utilizing Fundus Autofluorescence in Clinical Practice
Fundus flavimaculatus is known for its characteristic deep yellow flecks across the posterior pole. On fundus autofluorescence, you will see mixed hyper- and hypofluoresce pattern as seen in image C. The newer flecks are hyperfluorescent due to increased lipofuscin in the RPE whereas the older flecks have a hypofluorescent pattern due to loss of RPE.
(A: dry AMD with geographic atrophy
B: chronic ICSC
D: AMPPE)
|
WHY BECOME AN ORS FELLOW?
By Bill Denton, O.D., F.A.A.O.
Chair, Membership Committee
At some point in your career, you realize you just may be coasting. Your knowledge has been limited to the journals you receive and attempt to read, and the conferences that may not be as fulfilling as they once were. You simply need a challenge that will add an extra dimension to your professional learning.
Fellowship in the Optometric Retina Society (ORS) can provide several benefits in addition to the initial challenge of qualifying for this honor. Plenty of perks accompany your induction, but the coolest part is being associated with a body of knowledge and resources which can help you in many other ways. It is not uncommon to receive weekly thought-provoking emails about challenging cases and treatment dilemmas. Some fellows like to share their awesome cases they have diagnosed, while others post their cases with hopes that other Fellows will suggest an alternative differential diagnosis. At times it is like a round-table of brainstorming, but through the use of modern technology. Fellowship has little obligation with a huge opportunity for professional growth.
If you are up to the challenge of becoming a Fellow of the ORS, feel free to peruse the details and application at www.optometricretinasociety.org. Advice can be given to assist you in your quest. Feel free to contact us.
|
SPONSOR NEWS


Editor
in Chief
Anna K. Bedwell, OD, FAAO
Co-Editor
Brad Sutton, OD, FAAO |
Journal
Reviewers
Jared Staats, OD
Senior Graphic Designer
Matt Egger
|
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|