| |
Volume 15, Number 1 |
April 2019 |
|
|
Inside
This Issue |
|
|
|
|
|
This e-newsletter is provided free to doctors through industry support from |
 |
| |
FROM
THE DESK OF THE EDITOR
Spring is in sight and March Madness is in full swing. But in a teaching setting like mine, March is quite the opposite of madness. I practice in a satellite clinic of an optometry school. So this time of year, I am working with fourth-year students who are graduating in about a month and a resident who is 75% of the way through residency. Instead, for me March marks the calm before the storm that will arrive as brand new fourth-year students enter our clinic in May. From a teaching perspective, this time of year is very rewarding to see students successfully wrap up their four years and head out into the workforce representing our next generation of optometrists.
This gets me thinking about our future generation of ODs and the impact opening more optometry programs, as applicant numbers remain stagnant, will make on our field. Are we diluting the profession? Will these graduates successfully represent the profession? Regardless of your opinion, there is not much that can be done. At least in teaching, I can have an impact on making these graduating students as prepped and prepared as possible, which I guess in a sense is maddening and stressful. No pressure, right?
In other news, planning for the next ORS annual meeting, Retina Update 2019, is already underway by members Mohammad Rafieetary and Steve Ferrucci. Set your calendars to get up to 11 CE hours in sunny Scottsdale, Dec. 6 to 7. Who couldn’t use an escape to Arizona in December to hear the latest in posterior segment disease? More details to come in the next newsletter.
Lastly, just a reminder that we are always welcoming new members to join our group. If you have any interest in learning more, please visit our website, https://www.optometricretinasociety.org/join for details on how to become a fellow.
Anna Bedwell, OD, FAAO
Editor-in-Chief
PRESIDENT'S MESSAGE
Sadly, it’s time to say good bye to my dear friend Steven Ferrucci, OD. No, he’s not dead thank goodness, but he is moving on to one of the best positions in any organization: immediate Past President. Thank you Steve for all of the tremendous effort you put in to serving as President. I will be taking over as President and attempting to fill a large role that was so wonderfully performed by Steve and all of his predecessors. Thankfully, I will not be without outstanding help and wise counsel from Steve, but also from Julie Torbit as Vice President, Mohammed Rafieetary as Secretary and Chris Suhr as Treasurer. With the combined experience, knowledge and wisdom of these fine individuals, as well as, all others serving on the various committees and the rest of fellows, I feel that the ORS is in good hands. This is not a job that can or should be done alone.
As I review the membership of the ORS, from the founding Fellows down to our newest member, I am humbled to be considered worthy of being President of the Optometric Retina Society. The list truly reads as the greatest of the profession and I’m honored to call you all friends and colleagues. I feel as if I am a child walking in the footsteps of giants, but as I consider the great potential of this collective group, I hope that I can live up to the quote of the great Sir Isaac Newton: “If I have seen further than others, it is by standing on the shoulders of giants.” I will seek the counsel of the giants among us and hope to move this society forward by standing on their shoulders and gaining a greater vision of where we need to go and what we need to do to more fully reach the potential of this great Optometric Retina Society.
To all of my friends and colleagues in the ORS, thank you for your support….I’ll need it.
Sincerly,
Jeffrey Austin, OD, FAAO
ORS President

YOU
MAKE THE DIAGNOSIS
Answer appears later in newsletter.
Answer appears later in newsletter.

Image Gallery
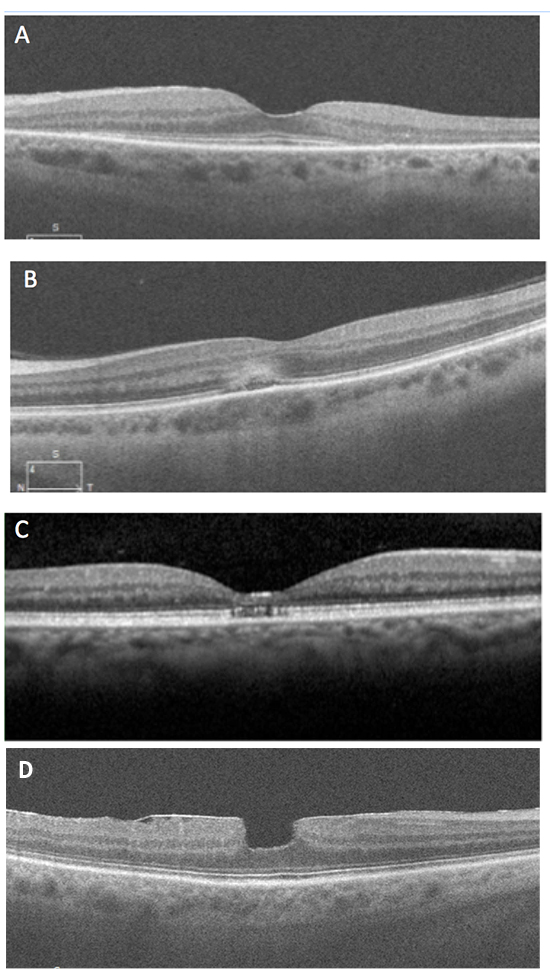
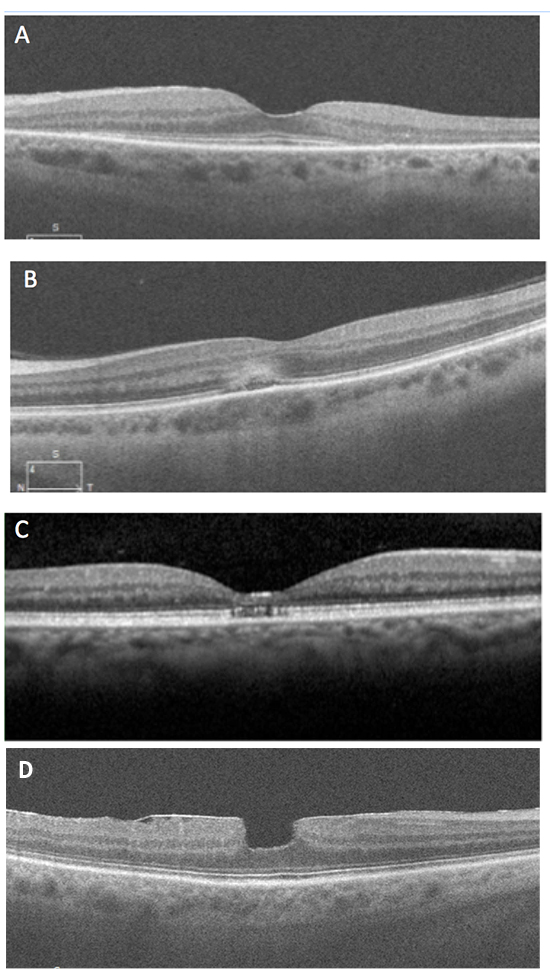
Which of the following OCT images represents hydroxychloroquine retinopathy?
Answer appears later in the newsletter.
|

JOURNAL
ABSTRACTS
En Face Optical Coherence Tomography Imaging of the Photoreceptor Layers in Hydroxychloroquine Retinopathy
Screening for hydroxychloroquine (HCQ) retinopathy has evolved over the years, with more emphasis relying on OCT and VF for early detection. The current standard for objective screening is using SD OCT B-scan images. In this particular study, the authors focused on the utility of en face OCT images in HCQ retinopathy screening.
This was a retrospective case review of 31 Asian patients (62 eyes) with evidence of HCQ retinopathy. All patients had objective evidence of retinopathy on swept-source OCT B-scan images and abnormalities on subjective HVF either 10-2 or 30-2. Additional testing was also considered such as FAF and ERG. Patients were categorized mild (32.3%), moderate (27.4%) or severe (40.3%) based on degree of photoreceptor loss and visual field defects. The presence of progression on OCT and/or FAF was assessed for in the 40 eyes with follow-up of ≥ 12 months.
En face imaging showed a beaten-bronze appearance in areas of photoreceptor loss with or without a hyporeflective demarcating border. En face imaging was 100% sensitive in detecting hydroxychloroquine retinopathy. This was better than FAF, which showed abnormalities (hyper- or hypofluorescence) in 53/62 eyes (85.5% sensitive). Progression was easier to analyze using en face in comparing direct images and quantifiable by measuring the area of intact photoreceptors. In correlation analysis, the area of central intact photoreceptors on en face showed statistically significant association as compared to 30-2 visual field indices of mean deviation, pattern standard deviation and visual field index (all p<.001).
This study suggested that en face OCT imaging might be complimentary with other screening tests in the evaluation for HCQ retinopathy. En face offers a one-dimensional image of the retinal plane to evaluate, whereas multiple OCT B-scan images must be analyzed for screening. This could also be helpful in progression analysis, as the central intact photoreceptor area is easier to visualize for change, and the intact area can be measured. Segmentation errors can be present with en face and must be considered with interpretation. It must be noted that this was a small study looking at patients of exclusively Asian ethnicity. As HCQ retinopathy presentation can vary, further study is necessary including analysis of various races.
Ahn SJ, Joung J, Lee BR. En face optical coherence tomography imaging of the photoreceptor layers in hydroxychloroquine retinopathy. Am J Ophthalmol 2019;199:71-81.
Evaluation of Obstructive Sleep Apnea Syndrome as a Risk Factor for Diabetic Macular Edema in Patients with Type II Diabetes
Obstructive sleep apnea (OSA) is more prevalent in patients with type II diabetes than the general population. As OSA lowers blood oxygenation levels, could it be antagonistic in the development of diabetic macular edema (DME)? These investigators sought to evaluate OSA as an independent risk factor for DME within a two-center, cross-sectional
case–control study.
The 99 patients with type II diabetes were separated into two groups based on +/- presence of DME. Patients with respiratory disease or previous OSA diagnosis were excluded. All patients were tested for OSA using Epworth questionnaire and an overnight polysomnography in hospital. The polysomnography recorded the apnea-hypopnea index (AHI), oxygen desaturation index, lowest saturation of peripheral oxygen (%SPO2 minutes) and cumulative time of SPO2 below 90% (CT90%). A positive OSA diagnosis was made with ≥5 AHI events/hour, moderate to severe OSA with ≥15/hour and severe OSA ≥30/hour.
Interestingly, for the DME+ group, the mean Epworth test score was 5.18 equating to a lower OSA risk compared with a score of 8.95 in the DME- group. This did not agree with polysomnography. The DME+ group had a higher AHI than the DME- group (43.95 vs. 35.18, p=0.034). Severe OSA was more prevalent in the DME+ group over the DME- group (71% vs. 50.8, p=0.049). In univariate analysis, CT90% was the only polysomnography value independently associated with DME. On secondary investigation, the group did not find a relationship between presence of diabetic retinopathy and OSA.
Overall, this study found a high correlation between severe OSA and DME. Further study is need to validate this conclusion and to determine impact of OSA treatment on DME.
Vié AL, Kodjikian L, Agard E, et al. Evaluation of obstructive sleep apnea syndrome as a risk factor for diabetic macular edema in patients with type II diabetes. Retina. 2019;39:274-80.
Autologous Retinal Transplant for Refractory Macular Holes: Multicenter International Collaborative Study Group
Even though macular hole (MH) surgery is generally quite successful, refractory MHs continue to be a struggle to determine proper technique for effective MH closure and to optimize final visual acuity. This report details a retrospective cases series of patients from four centers who had surgical repair with an autologous neurosensory retinal free flap. All patients had at least one prior surgery with internal limiting membrane removal and tamponade. Surgical technique varied minimally. The harvest site for the flap was in the mid-peripheral retina and at least calibrated in size to match the MH size. Tamponade consisted of either silicone oil, C3F8 gas or short-term PFC.
The case series consisted of 41 eyes that underwent the procedure and had over six months of follow-up. The mean inner opening aperture size was 825 ± 422.5 µm. Visual acuity improved in 15 eyes (36.6%), stayed stable in 17 eyes (41.5%) and decreased in 9 eyes (21.9%). Post-operative OCT showed complete MH closure in 36 eyes (87.8%). Of those 5 eyes that did not obtain MH closure, four had stable visual acuity and one declined. Significant post op complications included one eye with retinal detachment and one eye with vitreous hemorrhage. In seven eyes, retinal cystic spaces were noted on OCT months after surgery. This did not impact vision and no treatment was pursued as all resolved over a few months.
This paper reports on the largest case series of the autologous neurosensory retinal flap procedure for MH. Though retrospective and non-controlled, the surgical outcomes were encouraging of a safe, viable option for chronic large MH repair.
Grewal DS, Charles S, Parolini B, et al. Autologous retinal transplant for refractory macular holes: Multicenter International Collaborative Study Group. Ophthalmology. 2019 Jan 31. pii: S0161-6420(18)32595-8. doi: 10.1016/j.ophtha.2019.01.027. [Epub ahead of print].
Evaluation of Navigated Laser Photocoagulation (Navilas 577+) for the Treatment of Refractory Diabetic Macular Edema
There is reason to seek alternative to anti-VEGF treatment for diabetic macular edema (DME) considering the expense and potential serious risk of cerebrovascular incidents in elderly patients from chronic use of anti-VEGF medications. Laser has long been established to treat leakage from DME by sealing off microaneurysms. This retrospective study performed in Nahoya City University Graduate School of Medical Sciences evaluated the benefits of navigation laser photocoagulation (Navilas 577+ laser system) on patients with macular edema due to diabetes. The Navilas laser system (OD-OS GmbH, Telow, Germany) is a computer-based system combined with a wide-angle camera. This camera has eye-tracking laser, which is more accurate than traditional focal laser therapy and is used following preplanned treatment locations.
Twenty-five eyes of 21 patients with diabetic macular edema (DME) were evaluated and followed for a range of 7-16 months. All of the participants of this study had previous treatment either steroids or anti-VEGF injections. Laser was performed with the assistance of indocyanine green angiography (ICGA) in 21/25, fluorescein angiography (FA) in 3/25 and one with OCT angiography. Patients were evaluated at each visit with SD-OCT, along with BCVA, central macular thickness (CMT) and macular volume (MV). There was significant reduction of CMT and MV at follow-up. However, there was no significant improvement in BCVA. There were also no real side effects from laser treatment. Forty-four percent of eyes required additional navigated laser. After initial treatment, 9/25 did not need any retreatment due to macular edema resolving.
While this study focused on navigated laser treatment alone, other studies recently published show benefits to combined therapy of navigated laser with anti-VEGF agents by resolving DME and limiting amount of injections. This study had several limitations including its retrospective nature and a smaller patient base without a control group. More study should be done in evaluating the exact benefits of the navigated focal laser photocoagulation, but this study does show promising benefits of reducing macular thickness and potentially reducing the amount of injections needed in patients with DME.
Kato F, Nozaki M, Kato A, et al. Evaluation of navigated laser photocoagulation (Navilas 577+) for the treatment of refractory diabetic macular edema. J Ophthalmol. 2018; May 2;2018:3978514.
Sequential Changes in Hydroxychloroquine Retinopathy up to 20 years After Stopping the Drug: Implications for Mild vs. Severe Toxicity
Hydroxychloroquine (HCQ) has been an important drug used to treat patients with autoimmune and dermatoglocial disease. It is generally a safe medication, particularly with the screening tools for retinopathy available to date. The goal of this study was to observe progression of HCQ retinopathy once the medication was discontinued.
This study reviewed 13 patients, all with different stages of HCQ retinopathy with five to six years of sequential exam data. Some were monitored immediately after retinopathy was discovered while some presented years after the medication was already discontinued. Those with mild retinopathy showed patchy parafoveal damage of photoreceptors, while moderate retinopathy showed a ring of photoreceptor thinning with no RPE damage. Severe retinopathy showed damage to the RPE. Three patients exhibited mild stage retinopathy, two with moderate and eight with severe. The study used SD-OCT and FAF photos to monitor and measure foveal thickness and ellipsoid zone (EZ) line length. Unfortunately, dosage and duration of HCQ use was unknown. Severe cases showed progressive loss of EZ line of about 200 microns per year for up to 20 years following cessation of HCQ. The early and moderate cases were roughly stable when looking at the foveal thickness, while severe cases showed progressive thinning of up to 20 microns per year. Visual acuity was significantly different between the early and moderate cases versus the severe cases. Those with lesser damage maintained a visual acuity of 20/30 or better while the severe cases had VA close to 20/200 or worse. Similarly, central 10-2 visual fields showed stability on follow-up and mild loss in early and moderate cases, while severe cases showed pronounced central visual field loss.
Investigators found, in the small sample of patients, that after stopping HCQ, early and moderate damage due to HCQ retinopathy mostly remained stable. On the other hand, severe cases showed continued progression even up to 20 years after the patient stopped using HCQ. The mechanism of HCQ retinopathy progression is not well understood. The authors proposed that a potential compromise of cellular metabolic activity might cause severe HCQ retinopathy to mimic the continual degeneration found in genetic dystrophies. It is still unknown whether the damage in severe cases is due to direct toxicity from the HCQ drug to the RPE cells or to the photoreceptors. Regardless, this emphasizes the importance of proper screening and dosage monitoring of those on HCQ. This study showed the potential for HCQ retinopathy to progress even once the drug was stopped, reinforcing the importance of catching any damage as early as possible.
Pham BH, Marmor MF. Sequential changes in hydroxychloroquine retinopathy up to 20 years after stopping the drug: implications for mild versus severe toxicity. Retina. 2019 Mar;39(3):492-501.
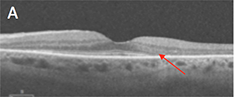
Peripapillary Retinoschisis in Glaucoma Patients
Though this research article is a few years old now, it is worth discussing because it covers an entity that often goes undetected in clinical practice: peripapillary retinoschisis in glaucomatous eyes. Peripapillary retinoschisis is present in up to 3-5% of eyes with glaucoma, but less than 1% of normal eyes. The schisis cavity involves the inner retina and the nerve fiber layer. It is often invisible or nearly invisible upon ophthalmoscopic exam, but can be seen on OCT scans. The schisis is typically contiguous with the optic nerve and radiates outward. It rarely involves the macula, so patients are often asymptomatic, and intervention is rarely indicated. The schisis can fluctuate with changes in intraocular pressure, and it can even resolve entirely over time. Some glaucomatous eyes with peripapillary retinoschisis exhibit visible acquired optic nerve pits, but many do not. An important factor to consider is the fact that changes in the schisis cavity over time can lead to changes in the measured RNFL thickness. A decrease in the size of the schisis may lead to a decrease in RNFL thickness measurement that does not truly represent progressive thinning of the RNFL.
Bayraktar S, Cebeci Z, Kabaalioglu M, et al. Peripapillary retinoschisis in glaucoma patients. J Ophthalmol. 2016;1612720.
Increased High-Density Lipoprotein Levels Associated with Age-Related Macular Degeneration: Evidence from the EYE-RISK and European Eye Epidemiology Consortia
There are many risk factors for developing age related macular degeneration, some of which are modifiable and some of which are not. European Researchers aimed to determine whether there might be a new, modifiable risk factor to consider. The study examined the lipid profiles of 4,730 individuals with early AMD, 2441 with late AMD, and 23,782 people without AMD. The data was mined from participants in 14 different studies in Europe. Total cholesterol, HDL, LDL and triglycerides were evaluated, and the presence/level of AMD was graded by fundus photograph. Elevated HDL levels were found to be associated with AMD, especially early AMD. This was particularly true in the case of high concentrations of extra-large HDL particles. Elevated total cholesterol, LDL and triglyceride levels were not found to be associated with AMD. Triglyceride and LDL levels were actually inversely related, with higher levels showing less accompanying AMD. So what does this information mean for clinicians? There are several things to consider. The association with AMD was essentially in the form of drusen formation, not pigmentary changes or advanced disease such as geographic atrophy or CNV. So basically, higher levels of HDL were associated with more drusen formation. It remains to be seen if elevated HDL is causative of retinal drusen formation, or is merely associated with it. With HDL generally being considered “good cholesterol” from a cardiovascular standpoint, and thus being desirable (though recent research has indicated that very high levels of HDL are not beneficial), it may be worth being aware of a possible link with increased drusen formation.
Colijn JM, den Hollander AI, Demirkan A, et al. Increased high-density lipoprotein levels associated with age-related macular degeneration: evidence from the EYE-RISK and European Eye Epidemiology Consortia. Ophthalmology 2019;126:393-406.
Estimating Medicare and Patient Savings from the Use of Bevacizumab for the Treatment of Exudative Age Related Macular Degeneration
It is well-known that Avastin is far less costly to administer than Lucentis or Eyelea when considering various anti-VEGF options. On average, Avastin costs around $60-$70 per dose, while Lucentis and Eyelea cost about $2,000. So what does this mean in the big picture? This report looked at the cost savings associated with Avastin use for exudative AMD compared to using the FDA approved therapies of Lucentis or Eyelea. Utilizing data covering the period from 2008 to 2015, the cost saving associated with Avastin use for AMD management was believed to be $17.3 billion, with Medicare savings of $13.8 billion, and patients or their secondary insurance saving $3.5 billion. Actual cost savings were even greater, considering that patients with Medicare Advantage replacement plans or private insurance were not included, nor were patients being treated for diabetic retinopathy or vein occlusions. Including patients with any insurance, and projecting the data out over 2016 and 2017 as well, the estimated savings jumps to a staggering $30 billion in the treatment of AMD alone.
Rosenfeld PJ, Windsor MA, Feuer WJ, et al. Estimating Medicare and patient savings from the use of bevacizumab for the treatment of exudative age related macular degeneration. Am J Ophthal 2018; 191:135-139.

|
ANSWER
TO "YOU MAKE THE DIAGNOSIS"
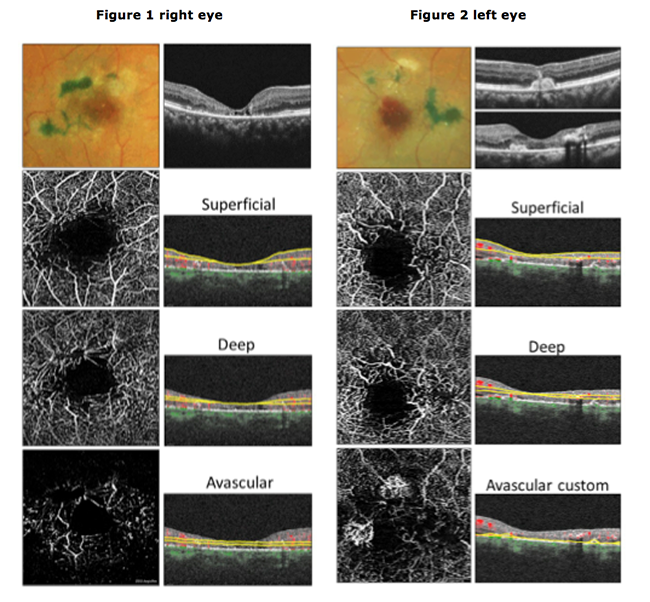
Macular Telangiectasia Type 2 Complicated by Subretinal Neovascularization OS
Introduction: Macular telangiectasia type 2 (MacTel2) is characterized by bilateral perifoveal telangiectatic capillaries manifesting in the fifth to sixth decade. Subretinal neovascularization (SRN) infrequently complicates MacTel2 and is likely retinal in origin.1 This case report highlights the utility of OCT angiography (OCTA) in detecting and imaging SRN in MacTel2.
Case Report: A 56 year-old Hispanic female complained of progressive vision decrease OU over the course of several years. Initial examination revealed visual acuities of 20/100 OD and 20/150 OS as well as perifoveal retinal opacity, mild crystalline deposits and temporal pigmented plaques OU. Additionally, superior perifoveal grayish subretinal thickening was noted OS. Structural OCT imaging revealed central outer retinal atrophy with associated subfoveal atrophic clefts OU. Two hyperreflective deposits (SRN) were visible superior and nasal to the fovea OS. The superior SRN membrane was associated with minimal adjacent RPE hyperpigmentation and had no associated fluid. The nasal SRN membrane had questionable adjacent subfoveal SRF. OCTA imaging revealed enlarged foveal avascular zones with irregular contour OU. Prominent dilated telangiectatic perifoveal capillaries, particularly temporally, were present OU. Custom avascular enface display OS revealed two SRN complexes superior and nasal to the fovea. Blunted venules of the retina were present, overlying both SRN membranes and appeared to anastomose with them. Fluorescein angiography was recommended to determine the exudative activity level of the SRN OS, but due to healthcare inaccessibility the patient was lost to follow-up until eight months later. OCT findings eight months later were unchanged OD. The nasal SRN membrane OS developed new, adjacent SRF although no morphologic change in the SRN membranes themselves were noted. Anti-vascular endothelial growth factor treatment of the SRN OS along with low-vision rehabilitation was recommended.
Conclusion: OCTA is a noninvasive technology that provides depth-resolved, high resolution microvascular detail of perifoveal telangiectasia in patients with MacTel2. This revolutionary tool is useful in detecting, quantifying and morphologically characterizing SRN membranes that may complicate MacTel2.
Carolyn Majcher
ORS Fellow
Figures:
1. Right eye. Color fundus photograph and structural OCT raster scan (top). 3mm macular OCTA superficial, deep, and avascular preset enface displays (left) with corresponding segmentation planes in yellow (right).
2. Left eye. Color fundus photograph and structural OCT raster scans through the superior parafoveal region and near the foveal center (top). 3mm macular OCTA superficial, deep, and customized avascular enface images (left) with corresponding segmentation planes in yellow (right). Two SRN membranes can be seen on the custom avascular enface image (bottom). Blunted venules of the retina can be visualized in the superficial and deep enface OCTA displays that overlie both SRN membranes and appear to anastomose with them.
1. Charbel Issa P, Gillies MC, Chew EY et al. Macular telangiectasia type 2. Prog Retin Eye Res. 2013 May;34:49-77.
|

IN THE
NEWS
 |
University of Alabama Researchers Determine New Genetic Biomarker for AMD
Researchers from University of Alabama in collaboration with University of Iowa reported a new genetic marker associated with AMD and delayed dark adaption. Their study, published recently in Ophthalmology, found that older adults with delayed dark adaptation are more likely to have high-risk genetic markers at chromosome 1 and 10, which correspond to CFH at chromosome 1 and ARMS2 at chromosome 10. In particular, they found that those with no clinical signs of AMD but with the ARMS2 A69S allele demonstrate delayed dark adaptation. This could be helpful to target pre-clinical treatment options.
|
 |
Janssen and MeiraGTx to Collaborate for Gene Therapy Programs
Janssen Pharmaceuticals, of Johnson & Johnson, and MeiraGTx announced plans for a global partnership and research agreement to develop gene therapies. The agreement allows Janssen an exclusive license to commercialize potential products for achromatopsia and X-linked retinitis pigmentosa within MeiraGTx’s inherited retinal disease portfolio. MeiraGTx will receive significant funding and a percentage of sales royalties from Janssen. The two companies will also collaborate to develop new products to address novel gene targets in the hope of developing new treatments for other inherited retinal diseases as well as new adeno-associated virus manufacturing technology.
|
 |
B+L Launches Sightmatters.com for Patients with AMD
In recognition of AMD awareness month in February, Bausch + Lomb unveiled a new educational online resource, SightMatters.com, for AMD patients. The website is designed to provide tips and tools for those with any stage of AMD. Larger fonts and distinct contrast are utilized to provide better visually impaired access. The site offers an opportunity for AMD patients to connect within a community for better support.
|
 |
Lutronic Vision Launches Preclinical Trial of R:GEN Laser for AMD
Lutronic Vision announced plans for a preclinical trial of its R:GEN™ laser to determine the laser’s efficacy and ideal setting for treatment of dry AMD. The study will take place at the University of Southern California with Stan Louie, PharmD, as lead investigator. R:GEN is a laser platform designed for selective retina therapy, specifically targeting RPE cells without causing photoreceptor injury. The R:GEN is designed to stimulate retinal repair rather than damage tissue.
|
 |
FDA Grants Fast Track Designation for NT-501 (Renexus) to Treat MacTel
Neurotech Pharmaceuticals announced that the FDA granted Fast Track designation for its product, Renexus (or NT-501), in the treatment of macular telangiectasia type 2 (MacTel). Renexus is a cell-based drug delivery entity that delivers ciliary neurotropic factor via human-based cells wrapped in a semipermeable fiber membrane device. Renexus has been shown in Phase II clinical trial to slow retinal degeneration in those with MacTel. Fast Track is a designation allowed by the FDA to accelerate promising drug development for serious conditions that have unmet medical need. There are currently no treatment options for MacTel.
|
 |
Researchers Develop Resistance-sensing Injector for Safer Drug Delivery
Researchers from Brigham and Women’s Hospital produced an intelligent-injector for tissue targeting (i2T2) capable of detecting resistance for safer medicine delivery to areas of delicate tissue, such as the suprachoroidal space. Their results were recently published in Nature Biomedical Engineering and include findings from testing on both extracted tissue and an animal model in the suprachoroidal, epidural and peritoneal spaces. Syringes have typically depended on the ability and experience of the operator to detect the injection site. The i2T2 rather senses a change in resistance when entering different tissue, then stops advancing and delivers the medication. This technology could have a broad range of application.
|
| |
|

|
IMAGE QUIZ ANSWER
The correct answer is A. Though uncommon, hydroxychloroquine (HCQ) can cause retinopathy in those taking the medication over many years or at a high dose. Technology now enables detection of retinopathy prior to visible funduscopic damage. On SD-OCT, HCQ retinopathy is noted by parafoveal loss of the ellipsoid zone, as demonstrated in image A (mod-severe retinopathy). The inferotemporal retina is often affected first. Wide-angle OCT scans are important in Asian patients as toxicity can occur further out near the arcades in these patients.
B: APMPPE C: solar retinopathy D: ERM with pseudohole
|
WHY BECOME AN ORS FELLOW?
By Bill Denton, O.D., F.A.A.O.
Chair, Membership Committee
At some point in your career, you realize you just may be coasting. Your knowledge has been limited to the journals you receive and attempt to read, and the conferences that may not be as fulfilling as they once were. You simply need a challenge that will add an extra dimension to your professional learning.
Fellowship in the Optometric Retina Society (ORS) can provide several benefits in addition to the initial challenge of qualifying for this honor. Plenty of perks accompany your induction, but the coolest part is being associated with a body of knowledge and resources which can help you in many other ways. It is not uncommon to receive weekly thought-provoking emails about challenging cases and treatment dilemmas. Some fellows like to share their awesome cases they have diagnosed, while others post their cases with hopes that other Fellows will suggest an alternative differential diagnosis. At times it is like a round-table of brainstorming, but through the use of modern technology. Fellowship has little obligation with a huge opportunity for professional growth.
If you are up to the challenge of becoming a Fellow of the ORS, feel free to peruse the details and application at www.optometricretinasociety.org. Advice can be given to assist you in your quest. Feel free to contact us.
|
SPONSOR NEWS

Editor
in Chief
Anna K. Bedwell, OD, FAAO
Co-Editor
Brad Sutton, OD, FAAO |
Journal
Reviewers
Daniel Bollier, OD
Senior Graphic Designer
Matt Egger
|
Review of Optometry® is published by the Review Group, a Division of Jobson Medical Information LLC (JMI), 11 Campus Boulevard, Newtown Square, PA 19073.
To subscribe to other JMI newsletters or to manage your subscription, click here.
To change your email address, reply to this email. Write "change of address" in the subject line. Make sure to provide us with your old and new address.
To ensure delivery, please be sure to add revoptom@lists.jobsonmail.com to your address book or safe senders list.
Click here if you do not want to receive future emails from Review of Optometry. |
|