 |
CTE has been depicted in both documentaries and mainstream cinema and continues to make headlines among news broadcasts and popular press, including Sports Illustrated, ESPN, National Geographic, Forbes and USA Today.2-4 Tragic suicides in high-profile athletes later found to have CTE (on autopsy)—including professional football players Dave Duerson and Junior Seau and, more recently, BMX rider Dave Mirra—have pushed this condition to the forefront.2-5
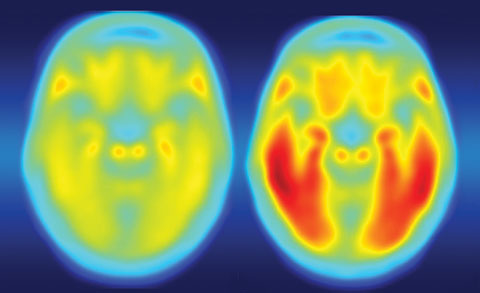 |
| Defective tau protein, as seen on the right positron emission tomography image, accumulates in the brains of patients with Alzheimer’s disease, Parkinson’s disease and CTE. Click image to enlarge. |
Sports and CTE
The clinical symptoms of CTE were first described nearly a century ago in boxers, and the disease was originally known as “punch drunk” or “dementia pugilistica.”6 It is only recently that research has associated modern sports, such as American football, soccer, ice hockey, motocross, BMX and rugby, with a similar deterioration.7,8Symptoms of CTE include changes in behavior (e.g., explosivity, violence, impulsivity) and mood (e.g., depression, suicidality, irritability), memory loss, diminished concentration, impaired motor functioning (e.g., parkinsonism, dysarthria, gait changes) and dementia.9
The clinical features of CTE are varied and typically manifest years or even decades after the initial episode of repetitive mTBI. Although the majority of patients report a history of concussions, this is not a prerequisite for diagnosis, suggesting that sub-concussive head injuries are sufficient to lead to the development of CTE.1
As with other neurodegenerative diseases, CTE can only be diagnosed with certainty by neuropathological examination of brain tissue.
Concussions and CTE
In its Practice Parameter, the American Academy of Neurology defines concussion as “trauma-induced alteration in mental status that may or may not involve loss of consciousness.”10 The terms concussion and mild traumatic brain injury refer to different injury constructs and should not be used interchangeably.
In the Zurich Consensus Statement on Concussion in Sport, researchers defined concussion as a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces.11
Several common features of concussion that may be useful for clinicians in defining the nature of a concussive head injury include:11
- Concussion may be caused either by a direct hit to the head, face or neck or a hit elsewhere on the body with an impulsive force transmitted to the head.
- Concussion typically results in the rapid onset of short-term impairment of neurologic function that resolves spontaneously.
- Concussion may result in neuropathological changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury.
- Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. In a small percentage of cases, however, post-concussive symptoms may be prolonged.
- Standard structural neuroimaging studies show no abnormality in concussion.
Overall, the number of years of exposure—not the number of concussions—is significantly associated with worse pathology in CTE.1,7,10 This suggests the chronic nature of head trauma, irrespective of concussive symptoms, is the most important driver of disease.1,12
Research also suggests CTE and continued exposure to head trauma is associated with other neurodegenerations, including Alzheimer’s disease.1
CTE, Concussions and the Eye
Concussions can cause any number of symptoms, including dizziness, nausea, headache, sleep problems, cognitive difficulties (i.e., feeling in a fog) and irritability.1,11Ocular symptoms can include visual blur, visual field loss, diplopia and photosensitivity.1,11
Research has found that CTE in particular can have a significant impact on ocular health. In a study of 10 eyes of deceased individuals with varying stages of CTE, researchers found pathology in the retina, mostly in the ganglion cell layer, throughout the different stages of the disease, with the most severe retinal pathology occurring in the most severe CTE stages.13 Ophthalmic sequelae associated with concussion and TBI may be sight threatening and visually debilitating.
The Tau of CTE
Alzheimer’s disease, Parkinson’s disease and now CTE have all been associated with tau proteins that have become defective.12,14,15 Tau proteins perform the important function of stabilizing microtubules. When these proteins become defective and fail to adequately stabilize microtubules, neuropathologies may develop.12Research suggests abnormal tau pathology in CTE occurs uniquely in those regions of the brain that are most susceptible to stress during trauma.7,9
In CTE, an accumulation of hyperphosphorylated tau (p-tau)forms within neurons and glia in a distinctive pattern. The abnormal tau accumulates in an irregular and patchy distribution that is perivascular and concentrated within the depths of sulci. In addition, the superficial cortical layers are preferentially involved compared with the deeper layers. This unique pattern of tau pathology is likely a result of force concentration during traumatic injury.1,12
CTE is therefore a tauopathy characterized by the deposition of p-tau protein as neurofibrillary tangles, astrocytic tangles and neurites in striking clusters around small blood vessels of the cortex, typically at the sulcal depths.
Patients with severely affected cases may show p-tau pathology throughout the brain.
Our next column will dig deeper into the possible ocular complications of CTE, along with testing protocols optometrists can incorporate into their practice to screen for this potentially devastating condition.
Dr. Wolter is in private practice in the Northeast region of Pennsylvania.
| 1. Stein TD, Alvarez VE, McKee AC. Concussion in chronic traumatic encephalopathy. Current Pain and Headache Reports. 2015;19(10):47. 2. Nowinski C. Head Games: Football’s Concussion Crisis. East Bridgewater, MA: Drummond Publishing Group; 2006. 3. Schwarz A. Dave Duerson Found to Have the Brain Trauma He Suspected. The New York Times. May 2, 2011. Available at www.nytimes.com/2011/05/03/sports/football/03duerson.html. Accessed February 2, 2017. 4. Fainaru-Wada M, Avila J, Fainaru S. Doctors: Junior Seau’s brain had CTE. ESPN.com. January 11, 2013. Available at www.espn.com/espn/otl/story/_/id/8830344/study-junior-seau-brain-shows-chronic-brain-damage-found-other-nfl-football-players. Accessed February 2, 2017. 5. Roenigk A. Doctors say late BMX legend Dave Mirra had CTE. ESPN. May 4, 2016. Available at www.espn.com/action/story/_/id/15614274/bmx-legend-dave-mirra-diagnosed-cte. Accessed February 13, 2017. 6. Martland HS. Punch drunk. JAMA. 1928;91:1103–7. 7. McKee AC, Cantu RC, Nowinski CJ, et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J Neuropathol Exp Neurol. 2009;68:709-35. 8. Miller K. Concussion knowledge in amateur motorcross. Electronic Theses & Dissertations. 2013:39. 9. Stern RA, Daneshvar DH, Baugh CM, et al. Clinical presentation of chronic traumatic encephalopathy. Neurology. 2013 Sep 24;81(13):1122-9. 10. American Academy of Neurology. Practice parameter: the management of concussion in sports. Neurology. 1997;48:581-5. 11. McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: 3rd international conference on concussion in sport. Zurich, Germany, November 2008. Journal of Athletic Training. 2009;44(4):434-448. 12. Verweiji BH, Muizelaar JP, Vinas FC, et al. Mitochondrial dysfunction after experimental and human brain injury and its possible reversal with a selective N-type calcium channel antagonist (SNX-111). Neurol Res. 1997;19:334-9. 13. Slick N. The ocular manifestations of chronic traumatic encephalopathy. ProQuest Dissertations & Theses Global. 2014. Available at http://search.proquest.com/docview/1560235964. Accessed February 2, 2017. 14. Lei P, Ayton S, Finkelstein DI, et al. Tau protein: relevance to Parkinson’s disease. Int J Biochem Cell Biol. 2010 Nov;42(11):1775-8. 15. Alves G, Brønnick K, Aarsland D, et al. CSF amyloid-beta and tau proteins, and cognitive performance, in early and untreated Parkinson’s disease: the Norwegian ParkWest study. J Neurology, Neurosurgery, and Psychiatry. 2010;18(10):1080-6. |

