 |
Fractures of the bony orbit typically present urgently, as the result of trauma. The threat of a neurological complication can induce a strong sense of anxiety in the patient, but an optometrist’s calm, thorough examination, and the appropriate ancillary testing, will ensure they receive the utmost care and achieve the best possible outcome.
By the Numbers
Epidemiologically, males in the adolescent (81%) and young adult (72%) age groups encounter orbital fractures significantly more often than their female counterparts.1,2 Most often, automobile accidents incite the trauma (45% to 54%).2,3 Falls (17.9% to 20.3%), assault (9.7% to 22.6%) and sports-related injuries (6.3% to 7.8%), round out the other major causes of the fractures.2,3 The bony structures most often succumbing to traumatic insult include those associated with the zygomatic complex: the arch, the maxillary buttress, the inferior orbital rim and the frontal articulation.2 After trauma, these patients will need a prompt and thorough ophthalmic examination.
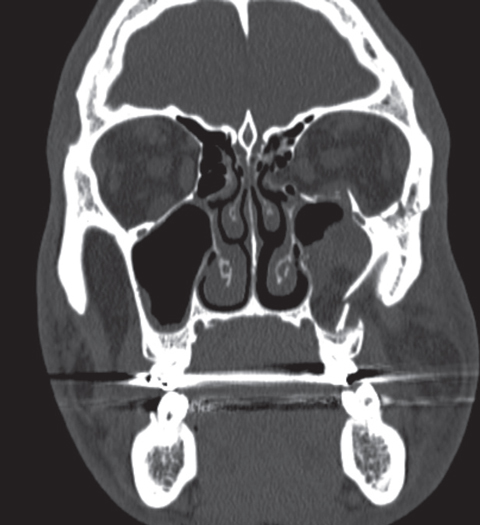 |
| Complex left maxillofacial fracture involving orbital floor, lamina papyracea, inferolateral rim and zygomatic arch status post facial trauma one week prior to scan. Orbital CT shows inferior rectus indentation and medial rectus tethering. |
Pathophysiology
The type and extent of each orbital fracture will determine the ophthalmic and related facial complications that arise from the trauma. Fractures typically affecting the orbit include wall, floor and roof blowout or trapdoor fractures, Le Fort types II and III fractures and zygomaticomaxillary fractures (formerly known as tripod fractures). The more rare orbital apex fractures have the potential to be visually devastating, due to traumatic optic neuropathies. The orbital floor and medial wall are fractured frequently in blowouts due to the relative delicacy of the thin ethmoidal and maxillary sinus bones.1,5 The most emergent of these fractures are trapdoor blowouts of pediatric orbital floors. In children, orbital bones are more pliable than in adults. Due to this malleability, an inferior blowout creates the trapdoor phenomenon as the inferior orbital contents can become trapped in the rebound of the supple bones.6 These cases are urgent and require surgical repair within 24 hours.6
1,000 Pictures’ Worth
Computed tomography (CT) scans are the standard for assessment of any orbital trauma. Before the advancements in CT scanning, radiologists mostly used standard film radiographs, or x-rays, to evaluate the extent of damage. However, with the greatly enhanced images provided by thin-slice CT scans and the technological ability to perform 3D reconstruction of bone, CT images undoubtedly provide the best assessment of the fractures. They can also be unparalleled in their ability to detect small fractures with a tear-drop sign—a herniation of orbital fat inferiorly through the orbital floor shaped like a tear drop—that may otherwise go unnoticed. With the relatively small spaces between each image and the extensive anatomy being studied, orbital CT scans with 3mm spacing often exceed 1,000 total images. A practitioner can compare the CT scans to clinical signs to establish a diagnosis and initiate comprehensive treatment plans.
Bones-a-Cracklin’
The presenting symptoms with orbital fracture vary from case to case. Depending on the force of the trauma and the resultant injuries, patients could have minimal ocular complaint or may present with significant symptomatology. Commonly, the fracture breaks down the bony barrier between the orbit and one of the facial sinus cavities and the resultant turbulent air flow creates a crackling sound or sensation known as crepitus.
While crepitus presents as a symptom, it can also be a sign if the examiner listens observantly. The trauma and sequelae can cause varying pain, diplopia, visual changes and hypesthesia. Intraocular complications can arise in upwards of 59% of cases, highlighting the utmost importance of a thorough exam.6 Ophthalmic signs and exam findings tend to correlate with the aforementioned symptoms. First, a decrease in visual acuity from various mechanisms—including corneal injury, anterior chamber reaction, visually significant hyphema, vitreous cells or hemorrhage (or both), traumatic optic neuropathy and commotio retinae throughout the macula (Berlin’s edema)—may occur.7
Patients will also frequently experience diplopia due to varying etiologies. Possible diplopic causes in orbital fracture include muscle entrapment, cranial nerve paresis, muscular hemorrhage, enophthalmos and orbital hemorrhage.8 Inferior rim fractures are commonly associated with hypesthesia, as the infraorbital nerve is lesioned, causing a loss of sensation in the corresponding facial structures.
Our examinations may uncover other signs, such as lid/orbital/conjunctival emphysema and ecchymosis, rhinorrhea or lid ptosis. The rhinorrhea must be observed quite carefully, especially in the rare cases of roof fractures, since the leak may be cerebrospinal fluid.9 Our findings, in combination with the symptomatology, CT scans and etiology of trauma, will determine the next steps.
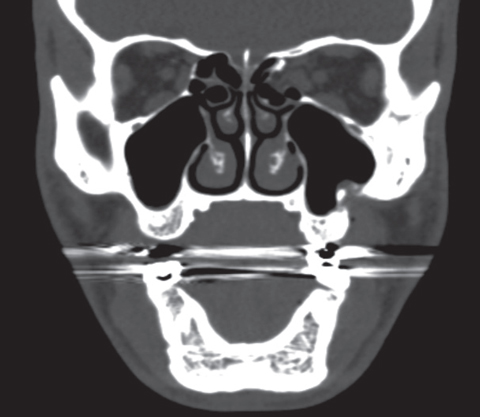 |
| This scan shows the same patient, four months following a post-orbital fracture repair. |
The Urgency of Observation
Once the appropriate work-up has been conducted and imaging reviewed in a timely manner, we can begin to make our soundest clinical judgments, recommendations and referrals. Our recommendations before surgical consult should focus on prophylaxis such as avoidance of nose-blowing, use of nasal decongestant spray—such as oxymetazoline-hydrochloride (Afrin) twice daily as needed for a maximum of three days and the slightly controversial oral antibiotics, usually amoxicillin-clavulanate (Augmentin) 250mg to 500mg TID for 10 days. As we know quite well, orbital cellulitis or abscess is one of the few true ocular emergencies. In the breakdown of the orbital-sinus barrier with these fractures, a direct conduit may be created for sinus microbiota to enter the orbital cavity. Once that cavity is breached, the potential for serious neurologic and systemic consequence increases dramatically.
Although seemingly emergent in our line of primary care work, these cases tend to be managed (or observed) rather conservatively by otolaryngologists. Some concerns that would indicate a need for surgical intervention include diplopia, entrapment of extraocular muscles (or any orbital contents), orbital abscess, 2mm or more of enophthalmos, or some combination. In addition, the previously mentioned pediatric trapdoor fractures should be quite urgently referred to surgery, as it is indicated within 24 hours.10 The surgical intervention may be multidisciplinary based on the structures involved, including otolaryngology and oculoplastics.
The proper primary evaluation and management for fracture patients remains well within the wheelhouse of the primary care optometrist. Through our studies, we have gained an extensive and intimate knowledge of the globe and its encompassing orbital structures. The surgeons will be counting on our thorough examinations, measurements and proper imaging to help guide them in surgical cases or to make initial determinations in regards to the need for surgical intervention. So long as we remain calm and comprehensive in our work-ups, we continue to ensure positive outcomes for our patients.
Dr. Dempsey is a primary care optometry resident at the Salem VAMC in Salem, Massachusetts.
1. Manolidis S, Weeks BH, Kirby M, et al. Classification and surgical management of orbital fractures: experience with 111 orbital reconstructions. J Craniofac Surgery. 2002;13(6):726-37. |

